Odovtos-International Journal of Dental Sciences (Odovtos-Int. J. Dent. Sc.), Online First, 2025. ISSN: 2215-3411
https://doi.org/10.15517/ac4b8809

https://revistas.ucr.ac.cr/index.php/Odontos
CLINICAL RESEARCH:
Comparative Effects of Prize Distraction and Conversation Distraction Behavioral Control Methods on Dental Pain and Anxiety of 3-7-Year-Old Children: A Clinical Trial
Uso de un método innovador de "distracción por premio" para reducir el dolor y la ansiedad
en niños durante tratamientos dentales: un estudio clínico aleatorizado
Maryam Rahmati DDS¹ https://orcid.org/0000-0002-4460-7387
Hamid Sarlak DDS, MS² https://orcid.org/0000-0003-4551-418X
Amir Almasi-Hashiani PhD3 https://orcid.org/0000-0003-4434-561X
¹Dentist, Private Practice, Arak, Iran.
²Assistant Professor, Department of Pediatric Dentistry, School of Dentistry, Arak University of Medical Sciences, Arak, Iran.
3Associate Professor, Department of Epidemiology, School of Health, Arak University of Medical Sciences, Arak, Iran.
Correspondence to: Hamid Sarlak - Dr.hamidsarlak@yahoo.com
Received: 2-V-2025 Accepted: 24-VII-2025
ABSTRACT: Management of pediatric patients’ dental pain and anxiety is a challenge. This study aimed to compare the effects of prize distraction (PD) and conversation distraction (CD) on dental pain and anxiety of 3-7-year-old children. This cross-over split-mouth randomized clinical trial was conducted on 64 systemically healthy children between 3-7 years with bilateral primary maxillary first molars requiring pulpotomy. The patients were randomly assigned to two groups. In the first group, PD was used in the first session for treatment of one randomly selected quadrant while CD was used in the second session for treatment of the other quadrant. This order was reverse in the second group. The pain and anxiety of patients were evaluated at the onset of each treatment session and during anesthetic injection by measuring their pulse rate (PR) as a physiological parameter, and using the Sound-Eyes-Motor (SEM) and the Wong-Baker Faces Pain Rating (WBFPR) scale. Data were analyzed by STATA 16 (alpha=0.05). Local anesthetic injection significantly increased the PR in both groups (P<0.05); however, this increase was significantly smaller in the PD group (P<0.001). Also, the WBFPR scale (P<0.002) and SEM (P<0.001) scores were significantly lower in the PD group than CD. Local anesthetic injection significantly increased dental anxiety of children in both groups despite the distraction methods. PD was significantly more effective than CD for reduction of dental pain and anxiety in 3-7-year-old children.
KEYWORDS: Pain; Dental anxiety; Dental care for children; Awards and prizes; Reinforcement, Psychology.
RESUMEN: El manejo del dolor y la ansiedad dental en pacientes pediátricos representa un desafío. Este estudio tuvo como objetivo comparar los efectos de la distracción por premio (DP) y la distracción por conversación (DC) sobre el dolor y la ansiedad dental en niños de 3 a 7 años. Este estudio clínico aleatorizado, tipo cross-over con diseño split-mouth, se llevó a cabo en 64 niños sistémicamente sanos, de entre 3 y 7 años, con primeros molares superiores temporales bilaterales que requerían pulpotomía. Los pacientes fueron asignados aleatoriamente a dos grupos. En el primer grupo, se utilizó la DP en la primera sesión para tratar un cuadrante seleccionado al azar, mientras que en la segunda sesión se utilizó la DC para tratar el otro cuadrante. En el segundo grupo, se invirtió el orden. El dolor y la ansiedad de los pacientes se evaluaron al inicio de cada sesión de tratamiento y durante la inyección anestésica, mediante la medición de la frecuencia del pulso (FP) como parámetro fisiológico, y utilizando la escala Sound-Eyes-Motor (SEM) y la escala de caritas de Wong-Baker (WBFPR). Los datos fueron analizados con el software STATA 16 (alfa=0.05). La inyección del anestésico local aumentó significativamente la FP en ambos grupos (P<0.05); sin embargo, este aumento fue significativamente menor en el grupo de DP (P<0.001). Asimismo, los puntajes en la escala WBFPR (P<0.002) y en la escala SEM (P<0.001) fueron significativamente más bajos en el grupo de DP en comparación con el grupo de DC. La inyección de anestesia local incrementó significativamente la ansiedad dental en los niños de ambos grupos, a pesar del uso de métodos de distracción. La DP fue significativamente más eficaz que la DC para reducir el dolor y la ansiedad dental en niños de 3 a 7 años.
PALABRAS CLAVE: Dolor; Ansiedad dental; Atención dental infantil; Recompensas y premios; Reforzamiento psicológico.
Introduction
Pediatric dentistry is a branch of dental science that addresses comprehensive dental care for children and adolescents (1). Despite the advances in this field of dental science, dental caries is still one of the most common chronic diseases in children (2). Dental fear and anxiety are highly prevalent among children and adolescents; one out of every five children experiences dental fear and anxiety, which can complicate the treatment process and compromise the outcome (1). Therefore, it is important for dental clinicians to establish a strong communication with children to increase their chance of attending subsequent dental visits (2).
Fear of pain and an unknown environment, presence of negative dental experiences, and presence of numerous sensory stimulants in the dental office setting such as the drilling sound and observing dental instruments can all contribute to dental anxiety (2, 3). Dental fear often leads to reluctance to seek dental care and can result in dental caries, pain, and infection, which further contribute to anxiety, creating a vicious cycle (4).
Several pharmaceutical and non-pharmaceutical methods are available for management of dental fear and anxiety of children. The pharmaceutical methods are often used for the management of high levels of anxiety while the non-pharmaceutical methods are commonly used for the management of low levels of anxiety (5). The non-pharmaceutical strategies used for reduction of dental fear and anxiety include verbal communication (6), the tell-show-do technique (7), positive reinforcement (5), and distraction. Distraction is commonly used to distract the patient’s attention from an unpleasant procedure and redirect it to focus on a more pleasant stimulus (8). According to the Gate Control Theory of Pain, the non-pharmaceutical methods such as gradual exposure to the stimulus, breathing maneuvers, and distraction block the pain signal transfer from the pain receptors to the brain, and decrease pain sensitivity as such (8, 9).
Verbal communication between dental clinician and pediatric patient can be considered as the most basic method of distraction [10]. Telling a story (11), listening to music (12), watching cartoons, and video games are among other methods of distraction (13). The novel non-pharmaceutical behavioral control methods such as virtual reality, and audio-visual equipment are also effective for distraction of children (14).
Positive reinforcement is another non-pharmaceutical behavioral control method, in which, the child receives a prize in response to his/her good behavior. It has been confirmed that this technique can effectively decrease the dental anxiety of children (5, 15). Positive reinforcement values and supports the dentist-child communication, relaxes the children, and encourages them to continue their good behavior (16).
Combined behavioral control techniques have also been proposed by some researchers. Bagherian and Sheikhfathollahi (17) introduced the cotton roll vibration technique as a combined distraction technique. The prize distraction (PD) technique is another novel technique introduced by Sarlak and Rahmati (18) in a case series study. In this technique, the clinician starts a warm and sincere conversation with the child focusing on prizes to increase the child’s motivation to receive a prize in response to showing a positive behavior. This technique is practiced right before a painful/anxiety causing stimulant, aiming to distract the children, increase their tolerance threshold, and decrease their anxiety level. It appears that combining several techniques with each other can increase their efficacy. The PD technique is a combination of distraction and positive reinforcement techniques, and is expected to benefit from the advantages of both techniques and maximize their efficacy. However, considering the novelty of the PD technique, it is still in need of further investigations.
Considering the previously reported positive results for the PD technique (18) and the fact that no previous clinical trial has assessed the efficacy of this technique, this study was undertaken aiming to compare the effects of PD and conversation distraction (CD) on dental pain and anxiety of 3-7-year-old children. The null hypothesis of the study was that the effects of PD and CD on dental pain and anxiety of children would not be significantly different.
Materials and Methods
This study was conducted at the Pediatric Dentistry Department of School of Dentistry, Arak University of Medical Sciences in 2023. The study protocol was approved by the ethics committee of the university (IR.ARAKMU.REC.1400.353) and registered in the Iranian Registry of Clinical Trials (IRCT20220315054300N1).
Trial design
A cross-over split-mouth randomized clinical trial was designed. Accordingly, each patient participated in the study twice and received both interventions (PD and CD). The results were reported in accordance with the Consolidated Standards of Reporting Trials.
Participants, eligibility criteria,
and settings
The inclusion criteria were genetically and systemically healthy children with optimal learning ability, age between 3 to 7 years, having bilateral primary maxillary first molars requiring pulpotomy and stainless-steel crown, no history of dental treatment or hospitalization, and having positive or definitely positive behavior according to the Frankl behavior rating scale.
The exclusion criteria were children with other carious teeth with a higher priority for treatment compared with primary maxillary first molars, presence of severe pain or any other condition necessitating prioritizing the treatment of one maxillary first molar over the other, which would no longer allow for randomization, and a sudden change in the child’s behavior during treatment such that the child’s behavior could no longer be assigned to the category of positive or definitely positive behavior.
The sample consisted of 64 eligible children.
Interventions
Written informed consent was obtained from all parents for participation of their children in the study and undergoing dental treatment. All children participated in four dental treatment sessions. The first session included clinical examination and radiography. The second session included the tell-show-do technique, treatment planning, and prophylaxis. In the third and fourth treatment sessions, a split-mouth design was adopted, such that for all children, the maxillary first molar of one randomly selected quadrant underwent treatment after behavioral control with PD while the maxillary first molar of the other quadrant was treated after behavioral control with CD. In the third treatment session, the children were randomly divided into two groups (n=30). Next, one maxillary quadrant was randomly selected by the sealed envelope technique. In the fourth treatment session, treatment of the other quadrant was performed after behavioral control with the second technique.
Group 1: PD in the first treatment session, and CD in the second treatment session.
Group 2: CD in the first treatment session, and PD in the second treatment session.
In the third and fourth treatment sessions, 20% benzocaine topical anesthetic gel (MasterDent, NC, USA) was applied at the injection site for 1 minute. Next, 2% lidocaine plus 1:80,000 epinephrine was administered by a short (16 mm) 30-gauge needle for infiltration anesthesia induction.
The pulse rate (PR) was used as a physiological parameter of dental anxiety of children, which was measured in the first session (PR1), second session (PR2), third treatment session (PR3), and fourth treatment session (PR4) as follows:
PR3A: It was measured 3 minutes after the child sat on the dental unit chair in the third treatment session.
PR4A: It was measured 3 minutes after the child sat on the dental unit chair in the fourth treatment session.
PR3B: It was measured during anesthetic injection in the third treatment session after implementing the behavioral control measure.
PR4B: It was measured during anesthetic injection in the fourth treatment session after implementing the behavioral control measure.
Considering the possible score tolerance of pulse oximeter during the measurements, the highest displayed PR value was recorded at each time point. Also, the pain level and anxiety of children during anesthetic injection in the third and fourth treatment sessions were quantified objectively by using the Sound-Eyes-Motor (SEM) scale, and subjectively by using the Wong-Baker Faces Pain Rating (WBFPR) scale.
SEM scale: The SEM table (Table 1) was used to score the pain experienced by children during anesthetic injection and following the initiation of distraction according to their behavior (sounds, eyes, and movements). A dental assistant determined and recorded the scores (19).
WBFPR scale: This scale was used for subjective quantification of pain experienced by children during anesthetic injection. The children were asked to express the level of pain they experienced during anesthetic injection (after the onset of distraction) by selecting a facial expression that best showed their pain experience, and the related score was recorded. Scores 0 to 5 indicated no pain, mild pain, moderate pain, severe pain, very severe pain, and extreme pain imaginable, respectively.
Subsequently, pulpotomy was performed and a stainless-steel crown was placed for maxillary first molars (Ds) similarly in the right and left quadrants after either PD or CD (cross-over design). Both behavioral control measures were started 20 seconds before picking up the dental anesthesia syringe and continued for up to 20 seconds after the 1-minute injection period (for a total duration of approximately 100 seconds). Infiltration anesthesia was administered by an experienced pedodontist without showing the syringe to the child.
In the PD technique, the dental clinician started a conversation with the child using the following phrases: honey, sweety, my boy, my girl, cutey, or my friend, and asked the following questions:
1. Have you ever received a prize?
2. Do you remember what it looked like?
3. Did you like it?
4. Do you know what a nice prize the boy/girl whose teeth I fixed before you won?
5. Do you want to get a nicer prize today?
6. Hey hero, did you know that we allow the children with good behavior to pick any prize they want?
7. Honey, do you know what nice prizes we have in the closet?
8. My friend, do you prefer a doll or a headdress (for girls)/a machine or a gun (for boys) as your prize?
In the CD technique, the dentist told a story about tooth microbes” Honey/my boy/my girl, sweety/my friend, do you know why microbes entered your tooth? When we eat sweets and chocolate, the microbes enter our teeth and are trapped there. If we do not brush out teeth very well, the microbes make a home in our teeth because they love sweets, and start eating our teeth. They become larger and chubby until they cause toothache”.
In both methods, the dental clinician’s tone and speech rhythm was as calm and slow as possible so that the children’s senses were fully engaged and they could visualize the sentences in their mind.
Outcomes (primary and secondary)
Dental pain and anxiety were the primary outcomes.
Sample size calculation:
The sample size was calculated to be 25 in each group according to a study by Jafarimofrad et al., (20) considering alpha=0.05, study power of 80%, the mean WBFPR scale score of 1.16 in the control group with a standard deviation of 0.8, and assuming that the PD behavioral control measure can decrease this value to 0.5, using STATA software. Considering the possible dropouts, 30 children were included in each group (PD-CD and CD-PD).
Interim analyses and stopping guidelines
None.
Randomization
The block randomization technique was used for randomization of patients. For this purpose, size 4 blocks were selected to determine the randomization sequence of patients as AB or BA. Also, for allocation of each behavioral control measure to each maxillary quadrant in the third treatment session, 60 identical envelopes were used; half of which contained a piece of paper coded L and the other half contained a piece of paper coded R. The envelopes were shuffled in the third treatment session, and each child randomly selected one envelope; letter R indicated treatment of the right quadrant while letter L indicated treatment of the left quadrant.
Blinding
The operator could not be blinded to the behavioral control measure of children. The observer who determined the SEM score and recorded the PR/min could not be blinded either since he could hear the dentist talking to children. However, the statistician who analyzed the data was blinded to the group allocation of the participants. Thus, the study had a single-blind design.
Statistical analysis
The Kolmogorov-Smirnov test was used to analyze the normality of data distribution. Accordingly, t-test and Chi-square test were applied for statistical analyses. The cross-over analysis was applied for maximum accuracy in statistical analysis (21). The treatment effect was analyzed to compare the efficacy of the two distraction methods. The sequence effect was analyzed to determine which sequence (PD-CD or CD-PD) was more effective, and the period effect was analyzed to find out which treatment session (first or second) was more effective. The carryover effect was also analyzed. All statistical analyses were carried out using STATA version 16 at 0.05 level of significance.
Table 1. SEM scale scoring.
|
Score |
Designation |
Sound |
Eyes |
Motor |
|
0 |
Comfort |
No sound indicating pain |
No eye signs of discomfort |
Hands relaxed, no apparent body tenseness |
|
1 |
Mild discomfort |
Nonspecific possible pain indication |
Eyes wide show of discomfort |
Hands show some tension |
|
2 |
Moderately painful |
Specific verbal complaint e.g. ow! Voice raised |
Watery eyes |
Random movement of arms/body grimace, twitch |
|
3 |
Painful |
Verbal complaint indicates intense pain |
Crying tears running down the face |
Movement of hands to make aggressive physical contact, pulling head away punching |
Results
Participant flow
A total of 70 children initially met the eligibility criteria and entered the study and were randomly assigned to 2 groups (n=35). In the PD-CD group, two patients did not show up for the fourth treatment session and the behavior of one child in the fourth treatment session was changed to completely negative according to the Frankl scale. Therefore, 32 children were finally analyzed in this group. In the CD-PD group, one child did not show up for the fourth treatment session, the behavior of one child in the fourth treatment session was changed to completely negative according to the Frankl scale, and the treatment plan of one patient was changed from pulpotomy to pulpectomy due to acute dental abscess. Thus, 32 children were finally analyzed in this group. Figure 1 shows the CONSORT flow-diagram of patient selection and allocation.
The mean age was 5.62±1.09 years in the PD-CD, and 5.65±1.18 years in the CD-PD group; the two groups had no significant difference in the mean age (P=0.913).
There were 19 females and 13 males in the PD-CD group, and 14 females and 18 males in the CD-PD group; the difference in gender distribution was not significant between the two groups (P=0.210).
The washout period was 16.25±6.13 days in the PD-CD group, and 13.98±4.13 years in the CD-PD group, with no significant difference (P=0.086). The time interval between the two treatment sessions ranged from 14 to 16 days in both groups.
Harms
No patients were harmed during the study.
Subgroup analyses
PR: Table 2 presents the PR in the first, second, and initiation of the third treatment session. As shown, the mean PR was not significantly different between the two groups in the first, second, or initiation of the third session (P>0.05). Comparison of PR1 (first session) and PR2 (second session) revealed a significant difference in both PD-CD (P<0.001) and CD-PD (P<0.001) groups, such that the PR significantly decreased in the second session compared with the first session in both groups. Comparison of PR2 and PR3A (initiation of third session) revealed a significant difference in PD-CD group, such that PR3A was significantly lower than PR2 in this group (P=0.014). However, this reduction did not reach statistical significance in the CD-PD group (P=0.058). Comparison of PR1 and PR3A revealed a significant difference in both PD-CD (P<0.001) and CD-PD (P<0.001) groups such that PR3A was significantly lower than PR1 in both groups.
As shown in Table 3, the increase in PR (as an indicator of anxiety) during anesthetic injection was significantly smaller in the PD group than the CD group. The treatment effect was also significant (P=0.001). The sequence effect was significant as well (P=0.002), indicating a significant difference between the order of receipt of the two distraction methods. However, the period effect was not significant (P=0.366), showing comparable therapeutic efficacy of the 3rd and 4th treatment sessions. The carryover effect on PR was not significant either showing that the treatment effect was not transferred from the 3rd session to the 4th session.
SEM scale: Table 4 shows the mean SEM score in the two groups. The treatment effect on the SEM score was significant (P=0.002), pointing to a significant difference between the two groups regarding the mean SEM score. The SEM score in the PD group was significantly lower than that in the CD group. The sequence effect (P=0.05), the period effect (P=0.24) and the carryover effect on SEM were not significant.
WBFPR scale: Table 4 shows the mean WBFPR scale score in the two groups. The treatment effect on the WBFPR scale score was significant (P<0.001), pointing to a significant difference between the two groups regarding the mean WBFPR scale score. The WBFPR scale score in the PD group was significantly lower than that in the CD group. The sequence effect (P=0.26), the period effect (P=0.015), and the carryover effect on the WBFPR scale score were not significant.
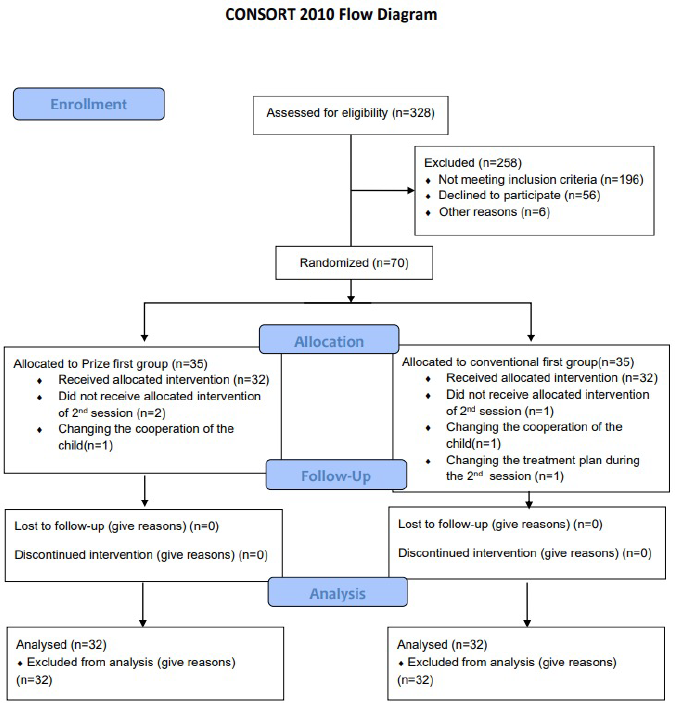
Figure 1. CONSORT flow-diagram of patient selection and allocation.
Table 2. PR in the first, second, and initiation of the third treatment session.
|
Pulse rate |
Group |
Mean PR/min |
Std. deviation |
P-value |
|
PR 1 |
1 (PD-CD) 2 (CD-PD) |
103.81 104.28 |
4.96 7.41 |
0.767 |
|
PR 2 |
1 (PD-CD) 2 (CD-PD) |
100.81 100.81 |
4.19 6.42 |
0.999 |
|
PR3A |
1 (PD-CD) 2 (CD-PD) |
100.00 100.31 |
3.86 6.12 |
0.808 |
Table 3. Mean difference in PRA (treatment onset) and PRB (during anesthetic injection) in the two distraction methods.
|
Group |
Period |
PRA |
PRB |
Difference PR |
|
PD-CD |
1 |
(3.86)100.00 |
(4.33)101.90 |
1.90 |
|
2 |
(3.99)101.46 |
(4.57)104.28 |
2.81 |
|
|
CD-PD |
1 |
(6.12)100.31 |
(7.15)104.68 |
4.37 |
|
2 |
(6.17)102.28 |
(6.73)105.09 |
2.81 |
|
|
Treatment effect= 0. 001 Period effect= 0. 366 Sequence effect=0. 002 Carryover effect=29.28% |
||||
Table 4. Comparison of the mean SEM and WBFPR scale scores between the two distraction methods.
|
Group |
Treatment session (period) |
SEM |
WBFPRS |
|
PD-CD |
1 |
(0. 63)0.28 |
(0.52)0.28 |
|
2 |
(0.73)0.68 |
(0.71)1.06 |
|
|
CD-PD |
1 |
(0.83)0.87 |
(0.83)1.00 |
|
2 |
(0.59)0.68 |
(0. 54)0.65 |
|
|
Treatment effect<0. 002 Sequence effect=0. 05 Period effect=0. 24 Carryover=29.28% |
Treatment effect<0. 001 Sequence effect=0. 26 Period effect=0. 015 Carryover=29.28% |
||
Discussion
This study compared the effects of PD and CD on dental pain and anxiety of 3-7-year-old children. PD is a novel technique composed of a combination of distraction and positive reinforcement, which has shown promising results (18). Cost-effectiveness is the main advantage of the PD technique. The two groups had no significant difference in the mean age, gender distribution, baseline PR, and washout period. The results showed a significant difference in PR in the second session compared with the first session, which can be due to the familiarization of children with the office environment and their subsequently decreased anxiety. The mean PR significantly decreased early in the third treatment session compared with the first session in the PD-CD group, which indicates that the tell-show-do technique was effective for anxiety reduction of children. However, this reduction did not reach statistical significance in the CD-PD group. In both groups, the mean PR early in the third treatment session was significantly lower than that in the first session, which can be due to the children’s acquaintance with the environment, effective dentist-child communication in the first session, and optimal efficacy of the tell-show-do technique practiced in the second session, all of which caused a significant reduction in anxiety level of children in the third session. In a cross-over clinical trial, Sadeghi et al. (22) compared the effects of distraction by an audio story and music on dental anxiety of children. They measured the PR and reported that frequent dental visits and the tell-show-do technique effectively decreased the anxiety level of children, which was in line with the present results. Also, Jafarimofrad et al. (20) compared audiovisual distraction and muted-video distraction for anxiety reduction of children by measuring their PR. Consistent with the present results, they showed that frequent dental visits, acquaintance with the dental office setting, and the tell-show-do technique effectively decreased the anxiety level of children.
The PR significantly increased during anesthetic injection compared with the value at the initiation of the third treatment session in both groups, showing that anesthetic injection increases the anxiety level of children probably due to the appearance of dental syringe, bitter taste of topical anesthetic agent, and pain felt by children during needle insertion and release of anesthetic agent into the tissue. This process increased the anxiety level of children despite distraction, showing that distraction was not completely successful to prevent anxiety in this step of the procedure. Consistent with the present results, Jafarimofrad et al. (20) reported that anesthetic injection increased the anxiety level of children despite the presence of audio-visual distraction. Similarly, Sadeghi et al. (22) showed that anesthetic injection significantly increased the PR as an indicator of anxiety, despite the audio distraction techniques. Nonetheless, the present results revealed that the increase in PR was significantly smaller in the PD method compared with CD. Also, the sequence effect was found to be statistically significant, indicating that prioritizing PD over CD would have a greater efficacy for anxiety reduction. The reason may be that implementing a successful method in the first step can gain the child’s trust. Since the period effect was not significant, the efficacy of the distraction methods did not depend on the treatment session. Unlike the present study, the treatment effect was not significant in the study by Sadeghi et al., (22) and both distraction methods were equally effective for reduction of dental anxiety of children in their study. Difference between their results and the present findings can be due to differences in the type of distraction methods. Jafarimofrad et al. (20) reported significantly smaller increase in PR following audiovisual distraction compared with muted video distraction. Their results cannot be compared with the present findings due to the differences in the adopted distraction methods.
The present results revealed a significantly lower SEM score in the PD group, indicating the superior efficacy of PD compared with CD for reduction of dental pain and anxiety during anesthetic injection in children. Bagherian and Sheikhfathollahi (17) compared the efficacy of the cotton-roll vibration technique and the conventional method of anesthetic injection for anxiety reduction in children in a split-mouth clinical trial. They used the Face, Head, Foot, Hand, Trunk and Mouth scale, which was almost similar to the SEM objective scale. Consistent with the present findings, they showed that the treatment effect was significant on the anxiety score of children, and the cotton-roll vibration technique was significantly more effective than the conventional method of anesthetic injection. Dahlquist et al. (23) evaluated the efficacy of a prize-based distraction technique. They used a touch and discover electronic toy that engaged the children in selecting a desired toy, and distracted them as such. They used the Observation Scale of Behavioral Distress, which is objective and comparable to the SEM scale used in the present study. They reported a significantly lower level of anxiety in the test group compared with the no-distraction control group. Their results were in agreement with the present findings, highlighting the optimal efficacy of interactive distraction for anxiety reduction. In the present study, the sequence effect on the SEM score was not significant, which was in agreement with the results of Sadeghi et al., (22) and Jafarimofrad et al. (20).
The present results revealed a significantly lower WBFPR scale score in the PD group than the CD group. The treatment effect was also significant on this score. The sequence effect was not significant, which was in line with the results of Sadeghi et al., (22) and Jafarimofrad et al. (20). The period effect was significant on the WBFPR scale score in the present study, indicating that the efficacy of distraction is significantly influenced by the period of distraction, which was in contrast to the results of Jafarimofrad et al. (20).
In total, the present results revealed significantly lower PR, SEM, and WBFPR scale scores in the PD than the CD group, showing that PD was significantly more effective than CD for reduction of dental pain and anxiety of children. Thus, the null hypothesis of the study was rejected.
This study had several strengths points. Using a combination of PR as a physiological parameter, SEM as an objective scale, and WBFPR scale as a subjective measure of pain and anxiety enabled more precise comparison of the distraction methods. Precise eligibility criteria and exclusion of patients with a previous history of dental treatment and negative experiences was another strength point which minimized bias and errors. Also, the present study appears to be the first clinical trial with a crossover split-mouth design on the effect of PD as a combined behavioral control method on dental pain and anxiety of children. This design eliminates the effect of inter-individual differences on the results and minimizes the risk of bias. Furthermore, the crossover analytical method was used for data analysis in the current study for maximum accuracy (21).
This study had some limitations as well. Strict eligibility criteria did not allow to recruit a larger sample size. Also, several treatment sessions resulted in some dropouts. Considering the obtained results regarding the optimal efficacy of the PD technique, future studies are required to verify the present findings and compare PD with other behavioral control methods. Furthermore, the efficacy of PD should be assessed for controlling pain and anxiety in other diagnostic and therapeutic procedures such as radiography and tooth extraction.
Conclusion
Local anesthetic injection significantly increased dental anxiety of children in both groups despite the distraction methods. PD was significantly more effective than CD for reduction of dental pain and anxiety of 3-7-year-old children.
Disclosure Statement: The authors do not have any financial interest in the companies whose materials are included in this article.
Conflict of Interest Statement: The authors also have no conflicts of interest.
AUTHOR CONTRIBUTION STATEMENT
Acquisition of data, and analysis and interpretation of data: M.R., H.S. and A.A.H.
Conception and design of the study: H.S.
Drafting the article: M.R., H.S. and A.A.H.
Final approval of the version to be submitted: M.R., H.S. and A.A.H.
References
1. Grisolia B.M., Dos Santos A.P., Dhyppolito I.M., Buchanan H., Hill K., Oliveira B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. International journal of paediatric dentistry. 2021 Mar; 31 (2): 168-83.
2. Horta T. Overcoming fear and anxiety in the dental office to promote oral health (Doctoral dissertation). 2022
3. Kebriaei F., Attarzadeh H., Foroughi E., Taghian M., Sadri S., Nemati M., et al. Dental Anxiety: The Prevalence and Related Factors among 7-14-year-old Children in Yazd, Iran. International Journal of Pediatrics. 2022; 10 (1): 15304-12.
4. Singh S., Mendiratta P., Saraf B.G., Sheoran N., Kapil D., Singh R. Miniature Pediatric Dental Office Model: A Tool for Assessing the Behavior of School-going Children in Dental Setting. Indian Journal of Dental Sciences. 2022; 14 (3): 116-20.
5. Hare J., Bruj-Milasan G., Newton T. An Overview of Dental Anxiety and the Non-Pharmacological Management of Dental Anxiety. Primary Dental Journal. 2019; 7 (4): 36-9.
6. Baldwin D., Williams A., McColl E. Top tips for paediatric dentistry-Part 1: examination and treatment planning for primary care. British dental journal. 2022; 232 (9): 596-8.
7. Kohli N., Hugar S.M., Soneta S.P., Saxena N., Kadam K.S., Gokhale N. Psychological behavior management techniques to alleviate dental fear and anxiety in 4-14-year-old children in pediatric dentistry: A systematic review and meta-analysis. Dental research journal. 2022; 19: 47.
8. D'Arro C. Harnessing the power of gate control: interventions for procedural pain and anxiety. The International Journal of Whole Person Care. 2022; 9 (1): 55.
9. Johnson M.H. How does distraction work in the management of pain?. Current pain and headache reports. 2005; 9 (2): 90-5.
10. Wells M., Mabry T.R., Christensen J.R., Nowak A.J., Townsend J.A. Pediatric Dentistry: Infancy Through Adolescence: Elsevier Health Sciences; 2019.
11. Amer H.W., Mohamed H.M.M.F., Ali S.A.O., Souilm N.A.M., Zaghamir D.E.F. Effect of Storytelling on Preoperative Anxiety and Fear among Children Undergoing Surgery. Egyptian Journal of Health Care. 2021; 12 (1): 938-47.
12. Janthasila N., Keeratisiroj O. Music therapy and aromatherapy on dental anxiety and fear: A randomized controlled trial. Journal of Dental Sciences. 2023; 18 (1): 203-10.
13. Venkiteswaran A., Halim R.A., Hasmun N.N. Effectiveness of Two Audiovisual Distractions for Paediatric Patients Undergoing Restorative Treatment. Journal of Multidisciplinary Dental Research. 2018; 4 (1): 33-41.
14. Alshatrat S.M., Sabarini J.M., Hammouri H.M., Al-Bakri I.A., Al-Omari W.M. Effect of immersive virtual reality on pain in different dental procedures in children: A pilot study. International Journal of Paediatric Dentistry. 2022; 32 (2): 264-72.
15. Rank R.C., Vilela J.E., Rank M.S., Ogawa W.N., Imparato J.C. Effect of awards after dental care in children's motivation. European Archives of Paediatric Dentistry: Official Journal of the European Academy of Paediatric Dentistry. 2018; 20 (2): 85-93.
16. Ridley-Johnson R., Melamed B.G. Behavioral methods and research issues in management of child patients. Anesthesia progress. 1986; 33 (1): 17-23.
17. Bagherian A., Sheikhfathollahi M. Children's behavioral pain reactions during local anesthetic injection using cotton-roll vibration method compared with routine topical anesthesia: A randomized controlled trial. Dental research journal. 2016; 13 (3): 272-7.
18. Sarlak H., Rahmati M. Prize-Distraction: A Combinatory Behavior Guidance Technique for Decreasing the Anxiety and Pain of Pediatric Dental Patients. Journal of Mashhad Dental School. 2022; 46 (1): 82-7.
19. Dhake P., Nagpal D., Chaudhari P., Lamba G., Hotwani K., Singh P. Buffered articaine infiltration for primary maxillary molar extractions: a randomized controlled study. Journal of dental anesthesia and pain medicine. 2022; 22 (5): 387-94.
20. Jafarimofrad S., Sarlak H., Nourmohammadi S. Is audio a mandatory component of multimedia distraction for reduction of pain and anxiety of pediatric dental patients? A split-mouth crossover randomized controlled clinical trial. Dental research journal. 2022; 19: 10.
21. Li T., Yu T., Hawkins B.S., Dickersin K. Design, Analysis, and Reporting of Crossover Trials for Inclusion in a Meta-Analysis. PloS one. 2015; 10 (8): e0133023.
22. Sadeghi M., Sarlak H., Nakhostin A., Almasi-Hashiani A. Which audio distraction technique is more effective for reduction the pain and anxiety of pediatric dental patients;" music" or" kids-story"? A randomized split-mouth crossover clinical trial. Journal of Psychosomatic Research. 2023; 168:111218.
23. Dahlquist L.M., Pendley J.S., Landthrip D.S., Jones C.L., Steuber C.P. Distraction intervention for preschoolers undergoing intramuscular injections and subcutaneous port access. Health psychology: official journal of the Division of Health Psychology, American Psychological Association. 2002; 21 (1): 94-9.
 Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.
Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.