Odovtos-International Journal of Dental Sciences (Odovtos-Int. J. Dent. Sc.), Online First, 2025. ISSN: 2215-3411
https://doi.org/10.15517/7kg2yp11

https://revistas.ucr.ac.cr/index.php/Odontos
CLINICAL RESEARCH:
Epidemiological and Clinical Characterization of Idiopathic Gingival Papillokeratosis with Crypt Formation (IGPCF)
Caracterización epidemiológica y clínica de la papilokeratosis gingival idiopática con formación de criptas (IGPCF)
Arturo Garrocho-Rangel DDS, MSc, PhD¹ https://orcid.org/0000-0001-9123-0300
Irma Yvonne Amaya-Larios PhD² https://orcid.org/0000-0002-3871-1102
Bruno Augusto Benevenuto-De Andrade DDS³ https://orcid.org/0000-0002-3259-606X
Arely Sánchez-Ibarra DDS⁴ https://orcid.org/0009-0000-0570-1031
Francisco Javier Tejeda-Nava DDS, MSc⁵ https://orcid.org/0000-0002-9330-6644
Amaury Pozos-Guillén DDS, MSc, PhD⁶ https://orcid.org/0000-0003-2314-8465
Saray Aranda-Romo DDS, MSc, PhD⁴ https://orcid.org/0000-0002-0379-9626
¹Pediatric Dentistry Posgraduated Program, Faculty of Dentistry, San Luis Potosí University, San Luis Potosí, S.L.P., México.
²Department of Dental Research, Centro Educativo de Humanidades (CEDHUM), Morelos, Mexico.
³Department of Oral Diagnosis and Pathology, School of Dentistry, Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil.
⁴Department of Diagnosis, Faculty of Dentistry, San Luis Potosí University, San Luis Potosí, S.L.P., México.
⁵Oral Radiology Clinic, Faculty of Dentistry, San Luis Potosí University, San Luis Potosí, S.L.P., México.
⁶Laboratory of Basic Sciences, Faculty of Dentistry, San Luis Potosí University, San Luis Potosí, S.L.P., México.
Correspondence to: PhD. Saray Aranda-Romo - sarayaranda@fest.uaslp.mx
Received: 18-VIII-2025 Accepted: 5-IX-2025
ABSTRACT: To clinically and epidemiologically characterize idiopathic gingival papillokeratosis with crypt formation (IGPCF) in a cohort of patients, aiming to enhance understanding and improve diagnosis and management of this rare condition. A cross-sectional study was conducted at the Diagnostic Clinic of the School of Stomatology, UASLP, between August 2022 and April 2023, including patients with complete electronic medical records containing demographic and medical information. Clinical diagnosis was supported by photographic documentation and cytological examination to rule out other pathologies. Group comparisons were performed with chi-square or Fisher’s exact tests. Logistic regression was applied to assess associations. A total of 7,163 patients were analyzed; the overall prevalence of IGPCF was 1.01% (95% CI: 0.79-1.26). Women had nearly a threefold higher likelihood of presenting IGPCF compared with men (OR=2.99, 95% CI: 1.76-5.10; p<0.05). No significant associations were found with age, smoking, alcohol use, or diabetes. Lesions were predominantly located in the maxilla (89.7%) and bilateral in 62.8% of cases. Mild gingival inflammation was observed in most evaluated cases. Clinically, lesions appeared as asymptomatic, pale-yellow, papillary plaques along the mucogingival junction. IGPCF is a rare, typically asymptomatic gingival condition with a distinct bilateral presentation in the maxillary gingiva, mostly affecting young adults. Proper identification is essential to prevent misdiagnosis. This study contributes the largest clinical dataset to date on IGPCF, reinforcing the need for standardized diagnostic criteria to support accurate clinical recognition and effective management.
KEYWORDS: Prevalence of Idiopathic Gingival Papillokeratosis; Oral lesions; Clinical diagnosis; Gingival mucosa.
RESUMEN: Caracterizar clínica y epidemiológicamente la papiloqueratosis gingival idiopática con formación de criptas (PGIFC) en una cohorte de pacientes, con el fin de ampliar la comprensión y mejorar el diagnóstico y manejo de esta rara condición. Se realizó un estudio transversal en la Clínica de Diagnóstico de la Facultad de Estomatología, UASLP, entre agosto de 2022 y abril de 2023, incluyendo pacientes con expedientes clínicos electrónicos completos que contenían información demográfica y médica. El diagnóstico clínico se apoyó en documentación fotográfica y examen citológico para descartar otras patologías. Las comparaciones entre grupos se realizaron con las pruebas de chi-cuadrada o la prueba exacta de Fisher. Se aplicó regresión logística para evaluar las asociaciones. Se analizó un total de 7,163 pacientes; la prevalencia general de PGIFC fue del 1.01% (IC 95%: 0.79-1.26). Las mujeres tuvieron una probabilidad casi tres veces mayor de presentar PGIFC en comparación con los hombres (OR=2.99, IC 95%: 1.76-5.10; p<0.05). No se encontraron asociaciones significativas con la edad, el tabaquismo, el consumo de alcohol o la diabetes. Las lesiones se localizaron predominantemente en el maxilar (89.7%) y fueron bilaterales en el 62.8% de los casos. En la mayoría de los casos evaluados se observó una leve inflamación gingival. Clínicamente, las lesiones se presentaron como placas papilares, asintomáticas, de color amarillo pálido, a lo largo de la unión mucogingival. La PGIFC es una afección gingival rara, típicamente asintomática, con una presentación bilateral distintiva en la encía maxilar, que afecta principalmente a adultos jóvenes. Su correcta identificación es esencial para evitar diagnósticos erróneos. Este estudio aporta el mayor conjunto de datos clínicos sobre la PGIFC hasta la fecha, reforzando la necesidad de criterios diagnósticos estandarizados para apoyar el reconocimiento clínico preciso y un manejo eficaz.
PALABRAS CLAVE: Prevalencia de Papiloqueratosis Gingival Idiopática; Lesiones oral; Diagnóstico clínico; Mucosa gingival.
INTRODUCTION
The uncommon and poorly understood condition known as gingival papillokeratosis (GP) has been typified by papillary lesions and hyperkeratosis on the gingival tissues. Although this clinical entity frequently manifests as a benign and asymptomatic condition, discomfort and functional problems may occasionally result. GP has been associated with hereditary factors, chronic irritation, and underlying systemic diseases, while the precise etiology is yet unknown (1,2). The global prevalence of gingival lesions, particularly papillokeratosis, poses a significant concern to clinicians within the field of dentistry. GI, characterized by keratotic lesions on the gingiva, has been observed in various populations (1). Recent clinical and epidemiological studies indicate that these lesions may be misdiagnosed as more severe conditions, underscoring the necessity for accurate characterization and understanding of their clinical implications (3).
Noonan et al. (1) presented the term “idiopathic gingival papillokeratosis with crypt formation” (IGPCF) to describe the pale-yellow plaques with a bluntly papillary morphology that are located bilaterally in the upper gingiva associated with the labial region along the mucogingival junction. With a reported mean age of 16±2.9 (range: 13-20) years and no sex predilection, the present study was the first well-documented group of seven IGPCF cases with clinicopathological findings affecting asymptomatic adolescents and young adults. In this same regard, Ide et al. (4) emphasized that a different name had already been used to publish this disease (i.e., “epithelial adnexal formation in the gingiva”). Other publication reported several features of this condition, including bilateral, symmetrical lesions that are only detected in the gingiva (5). Whether these lesions represent a unique entity, a gingival analog of a localized congenital epidermal nevus, or perhaps an acquired disorder brought on by local causes remains to be determined (1). Similarly, it is impossible to completely rule out the potential of a connection to the human papillomavirus due to the papillary structure of the lesion (5). There has also been speculation about a potential inherited susceptibility (6). However, the most recent research revealed no evidence of a familial predisposition (1). Microscopically, IGPCF has been observed, and it has been concluded that the gingival mucosa with parakeratosis and papillary acanthosis is linked with crypt-like multifocal epithelial invaginations without epithelial atypia (1).
The majority of the information that is currently available about IGPCF has been obtained from individual case reports or small patient series, making it difficult to assess the prevalence worldwide due to the scarce number of studies and reported cases (2). To date, no significant studies have systematically analyzed a considerable cohort of patients to better define the condition’s demographic distribution, clinical features, or potential risk factors. This study aims to provide a comprehensive clinical and epidemiological characterization of 79 patients diagnosed with IGPCF. By analyzing this cohort, we aim to identify common clinical presentations, demographic patterns, and possible contributing factors, thus contributing to the broader understanding of this rare condition and offering insight into more effective clinical management strategies. This study aims to complement the scarce knowledge about this pathology, thereby contributing to a more nuanced appraisal of its role in oral health.
PATIENTS AND METHODS
A cross-sectional epidemiological study was conducted at the Diagnostic Clinic of the School of Stomatology, Autonomous University of San Luis Potosí (UASLP), between 2022 and 2023.
The study population consisted of patients who attended the clinic during the specified period. Inclusion criteria: Male and female patients, aged 18-65 years, with complete electronic history. Exclusion criteria included participants who did not provide consent for their data to be used in research.
When the presence of IGPCF was identified, patients were invited to participate in the study by signing an informed consent form; for minors, authorization was signed by their legal guardian. They were informed about the nature of the lesion, as well as the risks and benefits of their participation in the study.
An individual patient history was taken; data were collected regarding their age, sex, existing diseases, medications, allergies, habits, and substance use; and extraoral and intraoral physical examinations were performed. This information was recorded on a data collection sheet. Subsequently, the characteristic of the lesion was documented by taking a clinical photograph and description concerning its localization, color, shape, texture, borders, and consistency. A differential clinical diagnosis was established concerning fungal or viral infection with an exfoliative cytology, and other plaque-like lesions were ruled out according to clinical definitions. For the identification of IGPCF, a prior calibration with an expert was conducted, achieving a kappa score >89%.
Statistical Analysis
Descriptive statistics were used to summarize the characteristics of the study population; categorical variables were expressed as absolute frequencies and percentages, while continuous variables were reported as means with standard deviations (SD). The comparisons between groups (with and without gingival papillokeratosis with crypt formation, IGPCF) were performed using the chi-square test or Fisher’s exact test for categorical variables, and Mann-Whitney U test for continuous variables.
Associations between IGPCF and sociodemographic, clinical, and behavioral variables were evaluated using logistic regression models. Results were expressed as odds ratios (OR) with 95% CI. A multivariate logistic regression analysis was performed to adjust for potential confounders (age, sex, cigarette smoking, alcohol use, and diabetes).
The study was conducted following the recommendations of the Declaration of Helsinki. All the selected participants signed a written informed consent form indicating their freedom and willingness to participate in the study after being fully informed of its objectives and specifics. The Institutional Ethical Committee approved the study protocol, patient information sheet, and informed consent forms (CEI-FE-002-023).
RESULTS
During the period from 2022 to 2023, a study was conducted on patients who attended the Diagnostic Clinic of the School of Stomatology at the Autonomous University of San Luis Potosí (UASLP). The analysis included the medical records of a total of 7,163 adults’ participants.
Of the 7,163 patients analyzed, 62.81% were female and 37.19% were male, with an overall mean age of 41.02 years (SD 17.31). Among patients with IGPCF, the mean age was 40.74 years (SD 16.18). The proportion of women was significantly higher in the IGPCF group (66.67%, 48/72) compared with the non-IGPCF group (36.89%, 2,616/7,091; p<0.05). Regarding comorbidities, no differences were found for gastrointestinal disease (16.42% vs 16.22%; p=0.965) or hypertension (14.93% vs 15.95%; p=0.82). In contrast, diabetes was less frequent among patients with IGPCF (4.17%, 3/72) compared with those without (11.72%, 831/7,091; p<0.05). With respect to lifestyle factors, current smoking was more common in the IGPCF group (33.33%, 24/72) than in the non-IGPCF group (18.47%, 1,310/7,091; p<0.05). Similarly, alcohol use was significantly higher in patients with IGPCF (40.28%, 29/72) compared with those without IGPCF (29.29%, 2,077/7,091; p<0.05). Table 1.
Overall prevalence of gingival papillokeratosis with crypt formation (IGPCF) in the study population was 1.01% (95% CI: 0.79-1.26), with no significant variation across age categories (p=0.869). Figure 1.
After adjusting for age, sex, cigarette smoking, alcohol use, and diabetes, women exhibited nearly a threefold higher likelihood of presenting IGPCF compared with men (OR=2.99, 95% CI: 1.76-5.10; p<0.05). On the other hand, no significant associations were found for the other variables included in the model, namely age categories, smoking status, alcohol consumption, and diabetes. Table 2.
Medication use and allergies. Thirty-five patients (44.87%) reported recent use (last 6 months) of one or more medications, with vitamins/supplements (37.14%), non-steroidal anti-inflammatory drugs (NSAIDs) (34.28%), and antihypertensive agents (31.42%) being the most prevalent. Seven patients (8.97%) had reported allergies or hypersensitivity, most commonly to antibiotics (42.85%), followed by foods and NSAIDs.
Lesion location and distribution. Most lesions were in the maxilla (89.74%), with only 10.25% occurring in the mandible. Males were more frequently affected in both locations. Bilateral presentation was observed in 62.82% of cases, whereas 37.17% were unilateral. Figure 2.
Orthodontic and oral hygiene practices. Only 7 patients (8.86%) reported current or previous use of orthodontic appliances, with a male predominance. Most patients (64.55%) used Colgate® toothpaste, with lesser usage of Crest® and Oral-B®.
Gingival index. Out of seven patients evaluated for the gingival index, 71.43% showed mild inflammation, and 28.57% had moderate inflammation, yielding an overall mean value of 0.98 (range: 0.5-1.9), indicative of mild oral inflammation. These findings provide an in-depth look at the demographic and clinical landscape of papilokeratosis in a diverse dental patient population.
Table 1. Sociodemographic characteristics of the patients who attended the diagnostic clinic of the Faculty of Dentistry during the period from 2022 to 2023..
|
Variable |
|
Total |
Without Gingival Papollokeratosis with Crypt Formation (IGPCF) |
With Gingival Papollokeratosis with Crypt Formation (IGPCF) |
p |
|
n |
7163 |
7091 |
72 |
||
|
Age |
Media (years) |
41.02 |
41.03 |
40.74 |
0.9047 |
|
|
Standar Desv. |
17.31 |
17.33 |
16.18 |
|
|
Sex |
% (n) |
% (n) |
% (n) |
|
|
|
|
Female |
62.81 (4499) |
36.89 (2616) |
66.67 (48) |
<0.05 |
|
Educational level |
% (n) |
% (n) |
% (n) |
||
|
|
Illiterate |
3 (0.04) |
0.04 (3) |
0 (0.0) |
<0.05 |
|
|
Reads or writes |
100 (1.40) |
99 (1.40) |
1 (1.39) |
|
|
|
Basic |
11.20 (802) |
11.20 (794) |
11.11 (8) |
|
|
|
Secondary |
21.12 (1513) |
21.18 (1502) |
15.28 (11) |
|
|
|
High school |
21.92 (1570) |
21.89 (1552) |
25 (18) |
|
|
|
Bachelor's degree |
36.13 (2588) |
36.17 (2565) |
31.94 (23) |
|
|
|
Technical degree |
5.91 (423) |
5.88 (417) |
8.33 (6) |
|
|
|
Postgraduate |
1.97 (141) |
1.99 (141) |
0 (0.0) |
|
|
|
Unregistered |
0.32 (23) |
0.25 (18) |
6.94 (5) |
|
|
Comorbidities |
|||||
|
Gastrointestinal |
16.22 (1161) |
16.22 (1150) |
16.42 (11) |
0.965 |
|
|
Hypertension |
15.94 (1141) |
15.95 (1131) |
14.93 (10) |
0.82 |
|
|
Diabetes |
11.64 (834) |
11.72 (831) |
4.17 (3) |
<0.05 |
|
|
Body Mass Index (BMI) |
% (n) |
% (n) |
% (n) |
||
|
BMI<18.5 |
Underweight |
3.17 (227) |
3.16 (224) |
4.17 (3) |
0.397 |
|
BMI=18.5 <=24.99 |
Normal or Healthy Weight |
26.90 (1927) |
26.99 (1914) |
18.06 (13) |
|
|
25 <=30 |
Overweight |
21.65 (1551) |
21.66 (1536) |
20.83 (15) |
|
|
BMI>30 |
Obese |
7.64 (547) |
7.63 (541) |
8.33 (6) |
|
|
|
Unregistered |
40.64 (2911) |
40.56 (2876) |
48.61 (35) |
|
|
Cigarette smoking |
% (n) |
% (n) |
% (n) |
||
|
Yes |
18.62 (1334) |
18.47 (1310) |
33.33 (24) |
<0.05 |
|
|
No |
81.38 (5829) |
81.53 (5781) |
66.67 (48) |
||
|
Alcohol use |
% (n) |
% (n) |
% (n) |
||
|
Yes |
29.40 (2106) |
29.29 (2077) |
40.28 (29) |
<0.05 |
|
|
No |
70.60 (5057) |
70.71 (5014) |
59.72 (43) |
||
|
Illegal drug use |
% (n) |
% (n) |
% (n) |
||
|
|
Yes |
2.04 (146) |
97.98 (6948) |
4.17 (3) |
0.199 |
|
|
No |
97.96 (7017) |
97.98 (6948) |
95.83 (69) |
|
|
Human settlement |
% (n) |
% (n) |
% (n) |
||
|
|
Rural |
5.51 (395) |
5.53 (392) |
4.17 (3) |
<0.05 |
|
|
Urban |
94.04 (6737) |
94.12 (6674) |
87.5 (63) |
|
|
|
Unregistered |
0.43 (31) |
0.35 (25) |
8.33 (6) |
|
|
Variable |
|
Total |
Without Gingival Papollokeratosis with Crypt Formation (IGPCF) |
With Gingival Papollokeratosis with Crypt Formation (IGPCF) |
p |
|
Main reasons for consultations |
% (n) |
% (n) |
% (n) |
||
|
|
Rutinal dental checkup |
44.91 (3217) |
44.92 (3185) |
44.44 (32) |
<0.05 |
|
|
Prophylaxis/tooth whitening |
10.74 (769) |
10.69 (758) |
15.28 (11) |
|
|
|
Pain and/or infection |
7.32 (524) |
7.33 (520) |
5.56 (4) |
|
|
|
Dental rehabilitation |
30.34 (2173) |
30.43 (2158) |
20.83 (15) |
|
|
|
Others |
6.52 (467) |
6.52 (462) |
6.94 (5) |
|
|
|
Unregistered |
0.18 (13) |
0.11 (8) |
6.94 (5) |
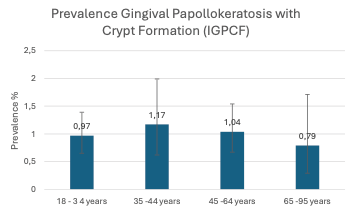
Figure 1. Prevalence of gingival papillokeratosis with crypt formation (IGPCF) by age group, with 95% confidence intervals.
Table 2. Factors associated with gingival papillokeratosis with crypt formation (IGPCF).
|
Odds Ratio (OR) |
(95% Conf. Interval) |
P |
|||
|
Age |
|||||
|
18 - 3 4 years |
1 |
||||
|
35 -44 years |
1.50 |
0.77 |
2.93 |
0.235 |
|
|
45 -64 years |
1.27 |
0.71 |
2.27 |
0.426 |
|
|
65 -95 years |
0.92 |
0.34 |
2.45 |
0.865 |
|
|
Sex |
|||||
|
Male |
1.00 |
||||
|
Female |
2.99 |
1.76 |
5.10 |
<0.05 |
|
|
Cigarette smoking |
1.57 |
0.90 |
2.74 |
0.111 |
|
|
Alcohol use |
1.10 |
0.64 |
1.89 |
0.729 |
|
|
Diabetes |
0.37 |
0.11 |
1.21 |
0.099 |
|

Figure 2. Clinical images of gingival papillokeratosis with crypt formation (IGPCF) observed in patients. A) An 18-year-old male patient with no relevant personal pathological history. He reports no known allergies or current pharmacotherapy. Currently undergoing orthodontic treatment. B) An 18-year-old female patient, systemically healthy, who denies a history of allergies and medication use. C) A 29-year-old male patient with a history of Human Papillomavirus (HPV) infection. He reports an allergy to apples and habitual alcohol consumption. D) A 25-year-old male patient who reports a diagnosis of gastritis and is under treatment with omeprazole. He presents with a history of substance abuse, including tobacco, alcohol, and cannabis (marijuana and CBD) use.
DISCUSSION
For the first time, the prevalence of IGPCF in the Mexican population is reported, which was 1.01%. Since no previous reports exist in the literature, these results are not yet comparable. However, this study establishes the foundation for future epidemiological research on this rare condition.
The literature on IGPCF is sparse, with few comprehensive reviews or clinical studies that address the epidemiological patterns, demographic characteristics, or clinical features of affected individuals. Existing reports typically focus on individual cases or a small cohort, limiting our understanding of the broader epidemiological trends and clinical variations in presentation (2,4). Furthermore, there is a lack of standardized diagnostic criteria and treatment protocols, which complicates the management and prognosis of this condition. Despite these challenges, early recognition and accurate diagnosis are essential to avoid unnecessary interventions and to provide appropriate care tailored to the patient's needs (1).
The existing literature primarily addresses broader categories of gingival lesions, often neglecting the unique characteristics of IGPCF (3). This oversight highlights the necessity for targeted studies that not only characterize these lesions but also investigate their potential associations with demographic variables such as age, gender, and underlying systemic conditions. Moreover, the implications of such lesions for oral health and their management in clinical practice warrant further exploration to enhance diagnostic accuracy and treatment outcomes (2).
A review of the literature revealed that while several studies have documented the presence of gingival lesions, there is a notable lack of focused research on IGPCF specifically (5). For instance, a retrospective analysis of 1,000 gingival lesions highlighted the predominance of reactive lesions, with non-reactive lesions being underrepresented (7). Furthermore, a study examining 500 patients indicated a high incidence of unclassified gingival papules, suggesting that further investigation should be performed into their histopathological characteristics (8). Despite these findings, the specific clinical features and epidemiological patterns of GI have not been thoroughly explored, representing a significant gap in the current understanding of oral lesions (2).
According to Noonan et al. (1), many oral epithelial lesions are keratotic and exhibit a papillary configuration; these include squamous papilloma, verruca vulgaris, localized juvenile spongiotic gingival hyperplasia, verruciform xanthoma, warty dyskeratoma, and, less commonly, acanthosis nigricans and oral epithelial nevi. All of these occur as discrete unilateral lesions. Those that form crypts are less frequent and include seborrheic keratoses of the perioral skin and acanthosis nigricans. Histopathologic examination of IGPCF reveals parakeratotic stratified squamous epithelium exhibiting a distinctive undulating papillary architecture with crypt formation and elongated, tapered rete ridges. The epithelial invaginations contained parakeratinaceous debris. The underlying connective tissue was densely collagenous without inflammation. Therefore, the clinical and histopathologic features of each lesion should be considered during the differential diagnosis process.
CONCLUSIONS
IGPCF is a rare, typically asymptomatic gingival condition with a distinct bilateral presentation in the maxillary gingiva, mostly affecting young adults. Proper identification is essential to prevent misdiagnosis. This study contributes the largest clinical dataset to date on IGPCF, reinforcing the need for standardized diagnostic criteria to support accurate clinical recognition and effective management.
AUTHOR CONTRIBUTION STATEMENT: Conceptualization and design: S.A.R., A.S.I. and F.J.T.N.; Literature review: A.G.R. and A.P.G.; Methodology and validation: S.A.R., B.A.B.D.A.and F.J.T.N.; Investigation and data collection: A.S.I. and B.A.B.D.A.; Data analysis and interpretation: A.G.R. and A.P.G.; Writing-original draft preparation: A.G.R.; Writing-review & editing: S.A.R., B.A.B.D.A. and A.P.G.; Supervision: S.A.R. and A.S.I.
REFERENCES
1. Noonan V.L., Woo S.B., Sundararajan D., Kabani S., Gallagher G. Idiopathic gingival papillokeratosis with crypt formation, a report of 7 cases of a previously undescribed entity: possible unusual oral epithelial nevus? Oral Surg Oral Med Oral Pathol Oral Radiol. 2017; 123 (3): 358-64. doi: 10.1016/j.0000.2016.10.018
2. Aranda-Romo S., de Arruda J.A.A., Nava F.J.T, Martínez L.E.M., Cavalcante I.L., de Andrade B.A.B. Idiopathic gingival papillokeratosis with crypt formation: A clinicopathological entity in the young population? Int J Dermatol. 2023; 62 (5): e291-3. doi: 10.1111/ijd.16579
3. Gambino A., Carbone M., Broccoletti R., Carcieri P., Conrotto D., Carrozzo M., Arduino P.G. A report on the clinical-pathological correlations of 788 gingival lesions. Med Oral Patol Oral Cir Bucal. 2017; 22 (6): e686-93. doi: 10.4317/medoral.21845
4. Ide F., Kikuchi K., Kusama K., Muramatsu T. An old report of idiopathic gingival papillokeratosis with crypt formation. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017; 123 (4): 515. doi: 10.1016/j.0000.2016.12.012
5. Betz S.J. HPV-related papillary lesions of the oral mucosa: A review. Head Neck Pathol. 2019; 13 (1): 80-90. doi: 10.1007/s12105-019-01003-7
6. Bennett J.S, Grupe H.E. Epithelial adnexal formations in human gingiva. Oral Surg Oral Med Oral Pathol. 1967; 23 (6): 789-95. doi: 10.1016/0030-4220(67)90371-4
7. Montazer Lotf-Elahi M.S., Farzinnia G., Jaafari-Ashkavandi Z. Clinicopathological study of 1000 biopsied gingival lesions among dental outpatients: a 22-year retrospective study. BMC Oral Health. 2022; 22 (1): 154. doi: 10.1186/s12903-022-02192-4
8. Khashabi E., Taram S., Saatloo M.V., Farjah G.H., Sharifi P., Gobaran Z.M. Epidemiologic and histopathological evaluation of unclassified gingival papules in Urmia, Iran. J Oral Maxillofac Pathol. 2023; 27 (1): 20-5. doi: 10.4103/jomfp.jomfp_122_21
 Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.
Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.