Odovtos-International Journal of Dental Sciences (Odovtos-Int. J. Dent. Sc.), Online First, 2025. ISSN: 2215-3411
https://doi.org/10.15517/d770js80

https://revistas.ucr.ac.cr/index.php/Odontos
NEW PERSPECTIVE ARTICLE:
An Update on Bulk-Fill Restorative Materials.
Myths, Facts and Guidelines for Predictable Clinical Application
Actualización sobre el estado de las resinas bulk-fill.
Mitos, realidades y guías para un uso clínico predecible
Marcelo Giannini¹ https://orcid.org/0000-0002-7260-5231
Alejandra Brenes Alvarado² https://orcid.org/0000-0003-1487-4123
Jorge Soto-Montero3 https://orcid.org/0000-0003-2257-7049
¹DDS, MSc, Ph.D., Full Professor, Department of Restorative Dentistry, Piracicaba Dental School, University of Campinas, Piracicaba, SP, Brazil.
²DDS, MS, MS, Ph.D. Associate Professor, Department of Pediatric Dentistry and Orthodontics, Universidad de Costa Rica, Montes de Oca, San José, Costa Rica.
3DDS, MS, MS, Ph.D. Full Professor, Department of Restorative Dentistry, Universidad de Costa Rica, Montes de Oca, San José, Costa Rica.
Correspondence to: Jorge Soto-Montero - JORGERODRIGO.SOTO@ucr.ac.cr
Received: 2-V-2025 Accepted: 2-VI-2025
ABSTRACT: Bulk-fill materials were developed to facilitate direct restorative procedures, mainly for deep and wide posterior cavities by allowing the placement of increments up to 4-5 mm thick. However, misinformation about the limitations on the technique used to place and polymerize these materials may impair achieving the topmost performance, because the mechanical properties may not be optimal at the deeper regions of the increment. Because the clinical performance of some materials varies according to the cavity depth, polymerization mechanism, chemical composition, this paper presents a general review of the materials available in the market, as a guide for the clinician, to help with the decision-making process and improve the predictability of the restorations made with bulk-fill materials.
KEYWORDS: Composite resins; Dental materials; Operative dentistry; Light curing.
RESUMEN: Los materiales restauradores de relleno en bloque, conocidos como "bulk fill" han sido desarrollados para facilitar la restauración directa, principalmente en cavidades amplias y profundas en el sector posterior, al permitir la colocación de incrementos de hasta 4-5 mm de grosor. Sin embargo, se han encontrado vacíos en la información disponible, sobre todo con relación a las técnicas recomendadas para la colocación y polimerización de estos materiales, lo cual puede reducir el rendimiento clínico, al no obtenerse las propiedades mecánicas deseables, especialmente en las regiones más profundas del incremento de resina. Debido a que el desempeño de las resinas de relleno en bloque puede estar influenciado por factores como la profundidad de la cavidad, el mecanismo de polimerización e inclusive la composición química del material restaurador, esta revisión presenta un panorama general de las características de los materiales disponibles en el mercado, con el propósito de orientar al clínico en el proceso de toma de decisiones, de manera que se mejore la predictibilidad del proceso restaurador, cuando se usan resinas de tipo "bulk fill".
PALABRAS CLAVE: Resinas compuestas; Materiales dentales; Operatoria dental; Fotocurado.
Introduction
Bulk fill restorative materials (BFM) simplify the restorative procedure as they reduce the repetitive placement of increments. The bulk curable resin-based BFM are recommended by manufacturers for placement and curing in increments of 4- to 5-mm thick (1, 2). Nonetheless, BFMs are not necessarily low shrinkage stress materials, as commonly thought, but materials that employ strategies to improve depth of cure and reduce polymerization shrinkage stress (PSS) development, (3) so the operator does not have to modulate it by incremental placement technique (3). Among the advantages of BFMs, is the reduction of the “chair time”, because fewer increments and light curing cycles are required to restore deep cavities (4. Also, there are fewer internal voids within the material bulk (4-6).
Placement techniques
A few representative examples of commercially available BFM based on different classification criteria are presented in Table 1. Of note, inclusion of a material in one category does not imply that it is excluded from the others, thus, there are flowable BFMs, that are also light-curable, resin-based bioactive materials. Therefore, the clinician should perform a careful analysis of the most appropriate material for each scenario, based on the desired results (1). A schematic representation of the different placement techniques, based on the consistency, application technique and depth of cure (4) of different BFMs is presented in Figure 1. In general, flowable consistency BFMs present lower mechanical properties than those of paste consistency, thus, flowable BFMs are not recommended for restoration of the occlusal surface of posterior teeth, which produces a requirement to combine flowable and paste BFMs (1,7). However, flowable BFMs can be used to fill most of the volume of the cavitary preparation, or as a liner in combination with paste consistency BFMs.
On the other hand, paste consistency BFM present mechanical properties comparable to conventional, incremental-fill resin-based composites (1). Thus, they can be used to restore the occlusal surface and in other load-bearing applications such as core build-up materials. Nonetheless, their application as final layer in direct restorations might be restricted because of the esthetic limitations of BFMs, because of the increased translucency and limited shade availability of these materials (3,7). Of note, evidence suggests that the use of different placement techniques does not result in a significant difference regarding operative time or presence of voids into the final restoration (4,6). Thus, BFMs appear as a restorative alternative that can be adapted according to the preferences and skills of the operator, while producing adequate results (4). The adaptability on placement techniques, as well as the reduction in the operative resulting from using fewer increments and polymerization cycles, and the potential bioactive effects of BFMs, (8) make them a promissory restorative material for dental specialties where the optimization of chair time is mandatory, such as pediatric dentistry (4).
Table 1. Summary of commercially available bulk-filling materials according to different classification criteria.
|
Criteria |
Type |
Manufacturer |
Commercial name |
|
By viscosity and application technique |
Flowable Resin-based composite |
Dentsply Sirona Tokuyama Dental Ivoclar-Vivadent Kulzer Shofu GC VOCO |
SureFil SDR Flow+ Estelite Bulk Fill Flow Tetric EvoFlow Bulk Fill Venus Bulk Fill Beautifil-Bulk Flowable G-ænial Bulk Injectable Admira Fusion X-base |
|
Paste consistency |
3M Oral Care Bisco Inc Ivoclar-Vivadent VOCO |
Filtek One Bulk Fill Restorative Reveal HD Bulk Tetric N-Ceram Bulk Fill GrandioSO x-tra |
|
|
Ultra-sonic condensation |
Kerr Dental |
SonicFill 3 |
|
|
Thermo-viscous |
VOCO |
VisCalor Bulk |
|
|
Self-adhesive |
Dentsply Sirona |
Surefil One |
|
|
By polymerization mechanism |
Light cured |
Ivoclar Vivadent FGM SDI Master-Dent VOCO |
Tetric EvoCeram Bulk Fill Opus Bulk Fill APS Aura Bulk Fill Master-Fil Bulk Fill X-tra fill |
|
Chemical/Self cured |
Bisco Inc. Ivoclar-Vivadent |
Bisfil 2B Cention N |
|
|
Dual cured |
Coltene Danville Silmet |
Fill-Up! BulkEZ ProFit Bulk |
|
|
By composition and filler |
Resin-based composites |
Voco Tokuyama Dental Ivoclar-Vivadent Kulzer Shofu GC |
Admira Fusion X-tra Estelite Bulk Fill Flow Tetric EvoFlow Bulk Fill Venus Bulk Fill Beautifil-Bulk Flowable G-ænial Bulk Injectable |
|
Glass ionomer |
GC |
Equia Forte Fil |
|
|
Resin-based Bioactive material |
Shofu Pulpdent Parkell VistaApex |
Beautifil-Bulk Restorative Activa BioActive Restorative Predicta Bulk Bioactive Re-Gen Bioactive Bulk Fill |
|
|
Fiber reinforced |
GC Pentron |
EverX BulkFill Posterior Alert |
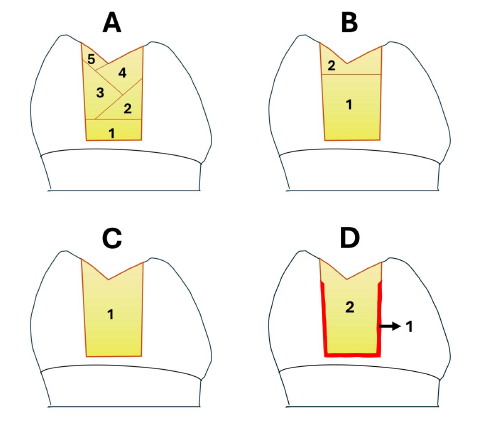
Figure 1. Schematic representation of a few techniques commonly used for restoration of deep, posterior cavities. A- Incremental technique: Several increments of resin-based composite with a thickness below 2 mm, are placed in a horizontal or oblique orientation and cured individually; B- The majority of the volume of the cavitary preparation is filled using a light or dual curable, flowable consistency bulk-fill composite, leaving an unfilled gap of 1- to 2 mm below the cavo-surface margin. Then, a paste consistency, conventional resin based composite is placed to finish the restoration on the occlusal surface; C- The complete volume of the cavitary preparation is restored using a single increment of paste-consistency bulk-fill composite with a thickness ranging from 4- to 6- mm; and D- The “Snowplow technique” a thin layer of flowable, light curable, resin-based bulk fill composite is applied as a coating on the internal walls of the cavity, without reaching the amelo-dentinal junction, and left uncured. Then, the complete volume of the cavitary preparation is restored placing a single increment of paste-consistency, bulk-fill composite with a thickness ranging from 4- to 6- mm over the lined cavitary walls, and the whole restoration is polymerized in a single light-curing cycle.
Polymerization
It has been reported that the heterogeneous light beams from light curing units (LCU) result in a non-uniform depth of cure in BFMs. This problem is enhanced in multiple-peak LCU, because of the lower penetration of the shorter wavelength violet light compared to light in the blue spectrum.(9,10) Therefore, when polymerization is made using a multi-wave LCU, the deeper part of the increment may not receive sufficient energy to be properly cured (1,2,11). To reduce the effects of light attenuation at the deeper regions of the BFM increment, research suggests that increasing the light exposure time results in a higher depth of cure for these materials, regardless of their photoinitiator composition or the emission spectrum of the light-curing unit used (2). Finally, in areas where the adequate placement or access of the LCU to the restoration is restricted, self or dual-curing materials could provide a more predictable result (1).
Technical drawbacks
Despite the proposed advantages of BFMs, there are a few limitations, such as the requirement of specific application devices, (7) a reduced variety of shades and limited esthetics, (7,12) compromised polymerization at depth because of the attenuation of the curing light as it passes through the material, (1,2) and poor internal adaptation because of PSS, (5) especially in high C-factor preparations. Nonetheless, better, or at least similar clinical performance is expected from BFMs compared to conventional resins composites (7). In sight of this considerations, a summary of common technical difficulties when using BFMs and the proposed strategies to overcome those limitations are presented in Table 2.
High PSS result in formation of marginal and internal gaps, microleakage around the restoration, cuspal deflection, tooth cracking, reduced bond strength, and lower mechanical properties of the restoration (3,5,7). Although the PSS of resin-based materials can be measured by laboratory methods, in a clinical scenario the PSS and its effects are influenced by restoration variables, such as cavity configuration, size and depth, as well as the selected adhesive system (5).
Table 2. Strategies to improve clinical performance of Bulk-fill materials.
|
Objective |
Do |
Why? |
|
Improve the depth of cure |
Check the manufacturer’s instructions for the BFM’s depth of cure. |
Resin-based BFM are designed to increase the depth of cure. Although adequate depth of cure of BFM has been reported,(2) manufacturers recommend different increment thicknesses, ranging from 4 to 6 mm. |
|
Make sure to irradiate the entire restoration when light curing the restoration. |
Width of the light beam is important when light curing a restoration made with a resin-based BFM, especially in large MOD restorations. Regions that are not covered with light may present inadequate polymerization (10,11). |
|
|
Verify the polymerization mechanism for the BFM. |
While light cured materials present a limited depth of cure (4 mm to 6 mm), dual cured materials may present unlimited depth of cure due to their chemical polymerization (1). However, they have limited working time. |
|
|
Light cure the BFM for the manufacturer’s recommended time. |
Depth of cure of the resin-based BFM materials may be prejudiced if the exposure time and radiant emittance are below the manufacturers recommendations (2,7). |
|
|
Reduce the effects of PSS. |
Isolate the operatory field, preferably with a rubber dam to reduce humidity. |
PSS increases when resin-based BFMs are exposed to humidity (3,5). Rubber dam isolation of the operatory field can control intraoral humidity and reduce PSS. |
|
Use a flowable BFM as cavity liner in high C-factor preparations. |
Flowable resin-based BFMs contain less fillers than paste-consistency BFMs. Although the lower filler content results in higher volumetric shrinkage, the resulting PSS is significantly lower than that of paste-consistency BFMs (3,5). |
|
|
Delay the light curing on dual cured BFMs |
Delaying light-activation of dual cured BFMs allows the polymer conversion to occur at a slower rate, enhancing the stress relief of the polymeric network, without a significant alteration of the mechanical properties (5). |
|
|
Use paste consistency resin-based BFMs for capping restorations partially filled with flowable BFMs |
The use of paste consistency resin-based BFMs as an occlusal layer over flowable BFMs results in similar bond strength to conventional resins and produces lower PSS at the enamel margin (3. |
Conclusions
Despite the operative advantages of BFMs, their use for restoration of posterior teeth requires conscious attention from the clinicians. Special care must be taken during placement in the proximal boxes of Class II restorations to ensure an adequate seal on the gingival margin, avoiding the presence of air voids and ensuring adequate curing of the material in hard to access regions. Also, adequate selection of the restorative material, in order to get the greater benefit from the consistency, curing or bioactive properties of each BFM.
Author contribution statement: Conception the manuscript: M.G.; Proofread the manuscript, discussion: M.G., A.B.A. and J.S.M.; Wrote the manuscript: J.S.M. All authors gave final approval and agreed to be accountable for all aspects of the work.
References
1. de Mendonça BC, Soto-Montero JR, de Castro EF, Pecorari VGA, Rueggeberg FA, Giannini M. Flexural strength and microhardness of bulk-fill restorative materials. J Esthet Restor Dent. 2021; 33 (4): 628-35.
2. Romano B., Soto-Montero J., Rueggeberg F.F.A.F., Giannini M., de Cássia Romano B., Soto-Montero J., et al. Effects of extending duration of exposure to curing light and different measurement methods on depth-of-cure analyses of conventional and bulk-fill composites. Eur J Oral Sci. 2020; 128 (4): 336-44.
3. Cerda-Rizo E.R., De Paula Rodrigues M., Vilela A.B.F., Braga S.S.L., Oliveira L.R.S., Garcia-Silva T.C., et al. Bonding interaction and shrinkage stress of low-viscosity bulk fill resin composites with high-viscosity bulk fill or conventional resin composites. Oper Dent. 2019; 44 (6): 625-36.
4. Soto-Montero J., Giannini M., Sebold M., De Castro E.F., Abreu J.L.B., Hirata R., et al. Comparison of the operative time and presence of voids of incremental and bulk-filling techniques on Class II composite restorations. Quintessence Int (Berl). 2022; 53 (3): 200-8.
5. Fronza B.M., Rueggeberg F.A., Braga R.R., Mogilevych B., Soares L.E.S., Martin A.A., et al. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent Mater [Internet]. 2015; 31 (12): 1542-51. Available from: http://dx.doi.org/10.1016/j.dental.2015.10.001
6. Hirata R., Pacheco R.R., Caceres E., Janal M.N., Romero M.F., Giannini M., et al. Effect of sonic resin composite delivery on void formation assessed by micro-computed tomography. Oper Dent. 2018; 43 (2): 144-50.
7. Pfeifer C.S. Polymer-Based Direct Filling Materials. Dent Clin North Am. 2017; 61 (4): 733-50.
8. Fronza B.M., Ayres A.P.A., Pacheco R.R., Rueggeberg F.A., Dias C.T.S., Giannini M. Characterization of inorganic filler content, mechanical properties, and light transmission of bulk-fill resin composites. Oper Dent. 2017; 42 (4): 445-55.
9. Palin W.M., Leprince J.G., Hadis M.A. Shining a light on high volume photocurable materials. Dent Mater [Internet]. 2018; 34 (5): 695-710. Available from: https://doi.org/10.1016/j.dental.2018.02.009
10. Soto-Montero J., Nima G., Rueggeberg F.A., Dias C.T.S., Giannini M. Influence of multiple peak light emitting-diode curing unit beam homogenization tips on microhardness of resin composites. Oper Dent. 2020 May 1; 45 (3): 327-38.
11. Shimokawa C.A.K., Turbino M.L., Giannini M., Braga R.R., Price R.B. Effect of curing light and exposure time on the polymerization of bulk-fill resin-based composites in molar teeth. Oper Dent. 2020; 45 (3): E141-56.
12. van Ende A., de Munck J., Lise D.P., Van Meerbeek B. Bulk-Fill Composites: A Review of the Current Literature. J Adhes Dent. 2017; 19 (2): 95-109.
 Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.
Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.