Odovtos-International Journal of Dental Sciences (Odovtos-Int. J. Dent. Sc.), Online First, 2025. ISSN: 2215-3411
https://doi.org/10.15517/cw0baw41

https://revistas.ucr.ac.cr/index.php/Odontos
LITERATURE REVIEW:
Digital Dentistry Applied in Orthodontics: A Bibliographic Review
Odontología digital aplicada en ortodoncia. Revisión bibliográfica
Macarena Garrido Díaz¹ https://orcid.org/0009-0006-3113-2534
Catalina Núñez Repenning² https://orcid.org/0009-0007-8092-4746
Camila Elgueta Droguett3 https://orcid.org/0009-0008-5202-000X
¹Faculty of Dentistry, Universidad de Valparaíso, Chile.
²Faculty of Dentistry, Universidad Católica, Chile.
3Faculty of Dentistry, Universidad Andrés Bello, Chile.
Correspondence to: Macarena Garrido Díaz - maca.garido14@gmail.com
Received: 14-I-2025 Accepted: 14-VII-2025
ABSTRACT: Developments in digital technologies have transformed dental practice, including orthodontics, by facilitating more accurate diagnoses and personalized treatments. This review aims to evaluate how digital dentistry has impacted diagnosis and planning in orthodontics, highlighting its precision and utility compared to traditional methods. A literature review was conducted following PRISMA guidelines in September 2024. Relevant studies were identified through searches on PubMed and SCOPUS using the keywords “( "orthodontic treatment" ) AND digital AND ( diagnosis OR planning )”. After the inclusion and exclusion criteria were applied, 10 articles were selected for final analysis. The reviewed studies emphasize that digital models are effective tools for orthodontic diagnosis and treatment planning, offering advantages such as reduced clinical time and improved accuracy in simulating dental movements. Technologies, including intraoral scanners and digital setups have shown to be especially effective in handling complex cases. Additionally, the use of CBCT combined with artificial intelligence has enhanced airway evaluation and provided more comprehensive diagnoses. However, the literature also highlights limitations associated with user expertise and variability among different technological systems. The findings of this review support that digital tools in orthodontics offer more precise diagnoses, better treatment planning, and an optimized patient experience. However, implementing these technologies requires overcoming challenges related to the learning curve and system standardization. Future research should focus on addressing these limitations and promoting a smoother integration of digital tools into clinical practice.
KEYWORDS: Orthodontic treatment; Digital; Diagnosis; Planning.
RESUMEN: El avance de las tecnologías digitales ha transformado la práctica de la odontología, incluyendo la ortodoncia, al facilitar diagnósticos más precisos y tratamientos personalizados. Esta revisión tiene como objetivo evaluar cómo la odontología digital ha impactado el diagnóstico y la planificación en ortodoncia, destacando su precisión y utilidad frente a métodos tradicionales. Se realizó una revisión bibliográfica siguiendo las directrices PRISMA en septiembre de 2024. Se identificaron estudios relevantes mediante búsquedas en PubMed y SCOPUS utilizando palabras clave “("orthodontic treatment") AND digital AND ( diagnosis OR planning )”. Tras aplicar criterios de inclusión y exclusión, se seleccionaron 10 artículos para el análisis final. Los estudios analizados destacan que los modelos digitales son herramientas efectivas para el diagnóstico y planificación ortodóncica, ofreciendo ventajas como reducción del tiempo clínico y mejor precisión en la simulación de movimientos dentales. La integración de tecnologías como los escáneres intraorales y setups digitales ha demostrado ser particularmente útil en casos complejos. Además, el uso de CBCT combinado con inteligencia artificial ha mejorado la evaluación de vías respiratorias y proporcionados diagnósticos más completos. Sin embargo, la literatura también resalta limitaciones asociadas con la experiencia del usuario y la variabilidad entre diferentes sistemas tecnológicos. Los hallazgos de esta revisión respaldan que las herramientas digitales en ortodoncia ofrecen diagnósticos más precisos, mejor planificación de los tratamientos y una experiencia optimizada para los pacientes. Sin embargo, la implementación de estas tecnologías implica superar desafíos relacionados con la curva de aprendizaje y la estandarización de los sistemas. La investigación futura debería centrarse en abordar estas limitaciones y promover una integración más fluida de las herramientas digitales en la práctica clínica.
PALABRAS CLAVE: Tratamiento ortodóntico; Digital; Diagnóstico; Planificación.
INTRODUCTION
Nowadays, the development of new technologies has significantly advanced dentistry, offering numerous benefits across all areas related to clinical practice and education (1).
Digital dentistry, together with artificial intelligence (AI), has revolutionized various domains of the field -such as digital radiography, model acquisition, and teledentistry- enabling greater accuracy in both diagnosis and treatment planning (2, 3).
Digital tools, including digital radiography and cone beam computed tomography (CBCT), are increasingly replacing conventional methods, improving both documentation and diagnostic analysis. Three-dimensional imaging enables personalized treatment planning through computer-aided design and manufacturing (CAD/CAM). The integration of digital models with specialized software facilitates treatment simulation and enhances communication with patients (4-6).
Orthodontics is no exception, as the success of treatment depends heavily on accurate diagnosis and precise planning. As such, the adoption of digital workflows is essential to increasing efficiency in orthodontic practice. Traditional techniques are being transformed through the use of modern technologies, enabling more effective diagnosis and treatment planning (3). A key development in this transformation is the automated detection of cephalometric landmarks on lateral cephalograms. These reference points, traditionally used to derive specific parameters, remain fundamental in the planning and evaluation of orthodontic treatment (3, 5, 7).
In the era of digital workflows, dentistry has been transformed by tools such as intraoral scanners, which have enabled professionals to replace traditional impressions and plaster models with high-precision virtual models. These innovative technologies are redefining how both diagnosis and treatment in orthodontics are approached, increasing accuracy and efficiency at every stage of care (4, 5).
Digital models have become essential tools in orthodontics due to their numerous advantages. They allow clinicians to integrate multiple data sources for treatment planning, with the ability to manipulate the model in any plane or orientation using zoom, rotation, and translation functions. Additionally, their durability and the ease of sharing images with other professionals and patients enhance collaboration and clinical monitoring.
These models also support detailed analysis of arch length discrepancies, accurate curvature measurements, and various orthodontic and surgical predictions. Furthermore, the integration of artificial intelligence enables the combination of diverse data types, expanding possibilities for three-dimensional analysis, diagnosis, and virtual treatment planning- ultimately improving efficiency and optimizing clinical workflows (5, 7-9).
In addition to these technical benefits, digital technologies also enhance the patient experience by providing a more personalized and interactive approach. With these tools, dentists can be more precise in diagnosis, prevention, and therapeutic intervention. Moreover, digital workflows can make treatment more convenient and accessible for patients (10).
The multiple facets of digital dentistry in orthodontics are reshaping the modern clinical landscape, allowing specialists to achieve more predictable and satisfactory outcomes. They also promote smoother communication across dental specialties.
For this reason, understanding the development of digital dentistry and its contribution to the diagnostic and treatment planning phases in orthodontics is essential in order to assess its precision and evaluate the outcomes reported in the literature.
OBJECTIVE
This review aims to identify the development of digital dentistry and evaluate its contribution to the diagnostic and treatment planning stages in orthodontics.
MATERIALS AND METHODS
During September 2024, a literature review was conducted based on the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). In the first stage, the study elements were identified, the PICO framework was developed (Table 1), and the research question was formulated: What is the impact of digital dentistry on diagnosis and treatment planning compared to traditional methods?
Inclusion Criteria
- Patients of all ages requiring orthodontic treatment.
- Studies published within the last 5 years.
Exclusion Criteria
- Patients who are not undergoing orthodontic treatment.
- Articles that do not mention diagnostic methods.
A search for the identification and selection of studies was conducted in the following databases: PubMed and SCOPUS, using the following keywords: "(orthodontic treatment) AND digital AND (diagnosis OR planning)" (Table 2). All selected articles were retrieved, analyzed, and reviewed by all authors.
The titles and abstracts of the retrieved studies were screened by the researchers, considering the inclusion and exclusion criteria described above. Full texts were obtained and reviewed in a second stage to confirm compliance with the criteria and to determine their eligibility for inclusion in this review.
RESULTS
The search yielded a total of 1.031 articles for evaluation. After removing duplicates, 691 records remained for title and abstract screening. Of these, 430 were considered relevant for full-text review. Following the application of eligibility criteria, 10 studies were included in this review (Figure 1).
The most relevant findings from each study are summarized in Table 3.
Table 1. PICO framework.
|
P Patient or Population |
I Intervention |
C Comparison |
O Outcome |
|
Patients requiring orthodontic treatment |
Digital dentistry |
Traditional methods |
The impact of digital dentistry |
Table 2. Search strategy.
|
Search strategy in PUBMED |
|
|
“( "orthodontic treatment" ) AND digital AND ( diagnosis OR planning )” |
763 Results |
|
Search strategy in SCOPUS |
|
|
“( "orthodontic treatment" ) AND digital AND ( diagnosis OR planning )” |
268 Results |
|
Total Results Obtained |
1.031 |
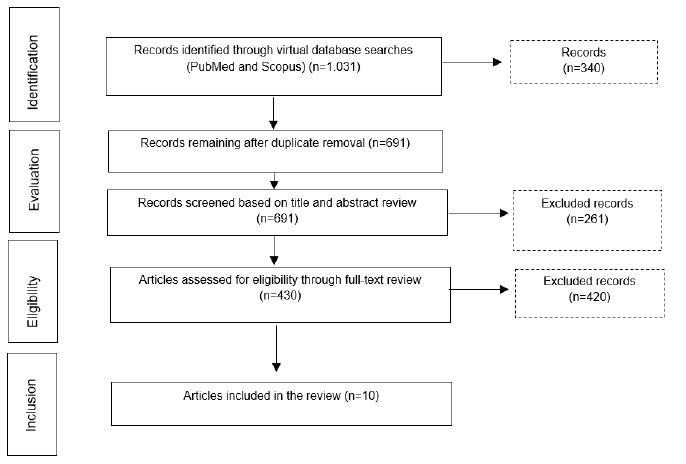
Figure 1. Results flowchart.
Table 3. Summary of main results.
|
Author |
Year |
Objetive |
Results |
|
Arathi Murugesan (6) |
2020 |
To evaluate the accuracy of digital models by comparing the measurements obtained from gypsum models, digital models derived from scanning the gypsum models, and direct in-traoral scans, with reference values obtained from direct intraoral measurements. |
No statistically significant difference was found in the measurements obtained using the four methods. |
|
Konrad Liczmanski (7) |
2020 |
To test the hypothesis that the dimensional differences between intraoral scans and conven-tional alginate impressions in mixed dentition are clinically irrelevant. |
The dimensional differences between intraoral scans and conventional alginate impressions in mixed dentition are clinically irrelevant for orthodontic purposes. In all clinical situations involving active treatment in mixed dentition, intraoral scans provide more detailed images and are less prone to errors. |
|
Nikolaos (8) |
2022 |
To examine the impact of the scanning strategy on the trueness and precision of impressions acquired with an intraoral scanner. |
The scanning strategy recommended by the manufacturer was statistically more accurate; however, the observed difference of 6-7 μm between the recommended strategy and alternative approaches is clinically insignificant. |
|
Derek Hou (9) |
2019 |
To evaluate whether the visualization of digital treatment simulations influenced orthodontic treatment planning decisions or the profession-als’ confidence in their selected plans. |
After reviewing the digital setups, a significant change in the treatment plan occurred in 9.2% of cases. These findings indicate that setups have a strong impact on treatment planning, especially for more complex cases. |
|
Aljaz Golez (10) |
2024 |
To investigate the factors associated with the risk of impaction and the need for surgical exposure. |
The results of the case-control study show that patients with impacted canines are more likely to have smaller maxillary dimensions, deep bite, hypoplastic lateral incisors, or rotated teeth adjacent to the canines. The presence of a persistent primary canine and a larger canine axis angle are local risk factors that increase the likeli-hood of canine impaction. Patients with impacted canines exhibited smaller maxillary volumes and surface areas. |
|
Mariya Balashova (11) |
2023 |
To explore potential applications of artificial intelligence for examining the upper airway and evaluating the reliability of automated assessments of cone beam computed tomography (CBCT). |
The field of artificial intelligence in orthodontic diagnosis may be valuable for examining the upper airway and holds significant potential. However, evidence regarding the use of artificial intelligence for upper airway assessment requires further research. |
|
Gusti Aju wahju Ardani (12) |
2020 |
To analyze the relationship between dentoalveo-lar heights and various vertical skeletal patterns in Class I malocclusion patients of Javanese ethnicity. |
Patients with Class I malocclusions in the Javanese ethnicity exhibit a significant relationship between dentoalveolar and vertical skeletal patterns. Upper posterior dentoalveolar height (UPDH) and/or lower posterior dentoalveolar height (LPDH) show a significant positive correlation with SN-MP, S-Go, Ar-Go, N-Me, and ANS-Me. The orthodontic correlation of decreased or increased facial height involved extrusion or intrusion of the anterior or posterior teeth in varying ways. |
|
Author |
Year |
Objetive |
Results |
|
Eun-ji Chung (13) |
2022 |
To evaluate the applicability and consistency of lateral cephalograms generated by cone beam computed tomography (CBCT) using artificial intelligence analysis. |
Conventional CBCT should not be used in general orthodontic practice due to the higher radiation dose. Lateral cephalograms, anteroposterior cephalograms, panoramic radiographs, and temporomandibular joint radiographs, which are generally required to formulate an orthodontic treatment plan, can be generated with our system from a single CBCT session. Although the radiation dose associated with a single CBCT session is higher than that of the four combined radiographs, since CBCT is performed only once, it can reduce patient exposure and discomfort while providing accurate 3D images. |
|
Samar M.Adel (14) |
2024 |
To evaluate the predictability of Invisalign SmileView for AI-based digital smile design compared to the actual outcomes of smile treatments. |
The Invisalign SmileView tool for smile simulation can be used with limited predicta-bility based on the conditions of the present study. More optimal lip lines, straighter smile arcs, and more ideal tooth display were achieved in the actual post-treatment outcomes compared to the initially predicted smiles. Five quantitative smile evaluation parameters-philtrum height, commissure height, smile width, buccal. corridor, and smile index-could be used as predictors. Only one qualitative parameter, the lip line, can be considered a reliable predictor for smile simulation. |
|
Aymar de Leotard (15) |
2024 |
To evaluate the reliability of digital orthodontic setups performed by orthodontists compared to those created by engineers from the 3Shape Design Service. |
Tooth Movements: Engineers from 3Shape® executed greater dental movements in rotation, tipping, buccolingual inclination, and mesiodistal translation compared to orthodontists. Secondary Measures: No significant differences were observed except in the number of displaced teeth, which was higher in the setups performed by engineers (3Shape: 15.32 vs. Orthodontists: 9.68). |
DISCUSSION
Digital Models
Study models are an essential tool for accurate diagnosis and treatment planning. According to the reviewed literature, comparisons of dental arch measurements obtained by four different methods-directly in the mouth, plaster models, digital models scanned directly from the mouth, and digital models derived from plaster casts-show some variations; however, these differences are not statistically significant (11).
Measurements taken directly in the mouth are considered the gold standard, as they are not subject to subsequent alterations. Although they present challenges such as the presence of saliva and limited space due to the patient’s tongue, they offer greater stability compared to plaster models, which may undergo expansion due to environmental conditions (11).
Direct measurements can only be performed on the anterior teeth, which limits their usefulness for diagnosis and treatment planning. In contrast, plaster and digital models can be used to evaluate the entire dental arch (11). Although both have been shown to be accurate replicas for measurement purposes, in this digital era, digital models represent a significant advancement. Their advantages include reduced clinical and laboratory time, as well as virtual treatment simulation; for these reasons, they are expected to become the most widely used models in the future (11,12).
Gavounelis and colls (13) demonstrated that scanning accuracy depends on three factors: the scanning strategy, the examiner, and repetition. Additionally, a positive correlation was found between the examiner and the strategy.
Although the manufacturer's recommended strategy is the most accurate, the overall impact of scanning accuracy based on strategy has not yet been fully determined. However, using an alternative strategy may result in slightly lower accuracy.
Regarding the examiner, differences were observed across studies. On one hand, better results were reported when the examiner had greater experience. In contrast, the study by Hou and colleagues (14) found that the examiner’s level of experience was not a determining factor. Nonetheless, despite these findings, the incorporation of a new digital system-such as an intraoral scanner-requires a learning process that involves a certain adaptation curve, even when the device is relatively easy to use (11).
Finally, it was observed that performing a second scan resulted in less accurate outcomes (13). It is worth noting that the studies reviewed analyzed models based on only one type of scanner. Therefore, future research should consider expanding this variable by including multiple scanner brands (11, 13).
Digitization has made significant progress by enabling the creation of digital setups, which offer advantages that plaster models could not provide. One key benefit is the ability to superimpose the digital setup onto the original models, allowing for a more precise calculation of the required movement for each tooth (14).
Hou and colls (14) revealed that the integration of digital setups leads to a significant shift in treatment planning, increasing confidence in the proposed plans. The ability to superimpose the setup onto the study model, accurately determine the incisal relationship, and assess the amount of interproximal reduction was among the most valued tools.
Digital setups are suggested to have a considerable impact on treatment planning, particularly in more complex cases. Their use is expected to expand as more practices adopt digital intraoral scanners and digital setup software continues to improve (14).
Assessment of Canine Impaction Risk
Digital dentistry has enabled the evaluation of the risk of canine impaction. In the study carried out by Golez, Vrcon, and Ovsenik (15), factors associated with the risk of canine impaction and the necessity for surgical exposure were determined through the measurement of digital models using specialized software, photographs, and lateral cephalometric radiographs. It was observed that patients presenting with deep bite, hypoplastic lateral incisors, and rotated adjacent teeth exhibited a significantly higher risk of impacted canines.
Moreover, local factors that increase the risk of impaction and the requirement for surgery were identified, including the presence of a primary tooth, palatal positioning of the canine, and a more pronounced angulation of its axis. Additionally, patients with impacted canines tended to have smaller maxillary volumes and surface areas (15).
Digital Dentistry and Artificial Intelligence in Orthodontic Diagnosis and Treatment Planning
CBCT and Airway Assessment
Artificial intelligence (AI) has proven to be a reliable tool for analyzing CBCT images, particularly in the assessment of the upper airway-a critical task in orthodontic treatment planning. AI allows for faster and more objective evaluations compared to conventional methods (16). Balashova et al. (17) emphasized that automated systems enable accurate visualization of the airway space and the detection of both total and minimum airway volume, which is useful in managing conditions such as adenoidal hypertrophy and mouth breathing. However, they noted the limitation of the study due to a small sample size (30 patients), suggesting that AI may be more suitable for initial screening rather than for the precise diagnosis of pathologies such as adenoidal hypertrophy.
In addition, information obtained from CBCT, when combined with AI, can generate detailed reports that identify potential pathologies, providing support in diagnosis and the selection of personalized treatment strategies. This enhances diagnostic efficiency and assists orthodontists and specialists in making informed decisions in complex cases.
Digital Cephalometry and Automated Cephalometric Analysis
Digital cephalometry generated from CBCT has also been evaluated in various studies, with models based on neural networks demonstrating over 90% accuracy in identifying anatomical landmarks (18).
Chung et al. (19) assessed the applicability and consistency of cephalograms generated by AI-based software such as OnDemand 3D and Invivo5. The results indicated no significant differences between measurements obtained from these tools and those from conventional cephalograms. This suggests that AI and CBCT-based tools can be effective in orthodontic diagnosis, particularly in pediatric and general orthodontics.
An additional benefit of using CBCT in cephalometric analysis is its ability to generate, from a single scan, multiple images required for diagnosis and treatment planning-such as lateral, panoramic, and temporomandibular joint radiographs. This can potentially reduce the patient's overall radiation exposure compared to acquiring multiple separate 2D radiographs. However, its indication should be made with clinical discretion, as the radiation dose of a single CBCT scan is higher than that of an individual 2D radiograph.
Digital Smile Design (DSD)
Digital Smile Design (DSD) has become a well-established tool in the planning of complex orthodontic treatments, particularly in multidisciplinary settings. Charavet, Bernard, Gaillard, and Le Gall (20) emphasized that DSD enables the analysis of facial, dental, and smile proportions, enhancing the predictability of final outcomes and facilitating communication among members of the interdisciplinary team. Additionally, the system’s reference lines provide valuable guidance for orthodontists in correcting aesthetic and functional discrepancies.
Furthermore, AI-based tools such as Invisalign SmileView have begun to explore digital smile simulations. According to Adel et al. (21), SmileView can predict key smile parameters such as philtrum height, commissure height, and smile width, although the predictability is limited. While certain qualitative parameters-such as the lip line-were considered reliable, others, such as the width of the maxillary canines, exhibited limitations.
Comparison of Tooth Movements
in Digital Setups
A recent study by De Leotard and Le Norcy (22) compared digital setups created by orthodontists with those designed by engineers from the 3Shape Design Service®, revealing key differences in tooth movements. The 3Shape® engineers performed greater movements in rotation, tipping, buccolingual inclination, and mesiodistal translation compared to the orthodontists. However, the practical impact on mild malocclusions was minimal, with the only notable difference being a higher number of teeth displaced in the 3Shape® setups.
These findings highlight the importance of establishing clear treatment objectives and considering overcorrection strategies when designing digital setups. For mild malocclusions, setups created by engineers may represent a viable alternative to those by orthodontists, although their reliability in more complex cases still needs to be evaluated.
CONCLUSION
The integration of digital models has transformed orthodontic practice by offering precision, efficiency, and flexibility in diagnosis and treatment planning. While direct intraoral measurements remain the gold standard due to their accuracy, digital models stand out for their ability to analyze the entire arch and facilitate virtual simulations, thereby reducing both clinical and laboratory time.
The accuracy of digital models depends on factors such as the scanning strategy, the examiner's experience, and the repetition of the procedure, highlighting the importance of proper training. Digital setups have enhanced treatment planning by increasing clinicians’ confidence and enabling the assessment of complex tooth movements.
In the diagnosis of conditions such as canine impaction, digital models and advanced tools like digital cephalometry have made it possible to identify risk factors and plan more effective interventions.
Digital dentistry, driven by artificial intelligence, is optimizing orthodontic diagnosis and treatment, promising a more precise and efficient future. Although challenges remain-such as the standardization of scanning strategies-its adoption continues to grow, transforming clinical practice.
Author contribution statement: Conceptualization and design: M.G.D.; Literature review: M.G.D. and C.E.D.; Methodology and validation: M.G.D.; Formal analysis: C.E.D.; Investigation and data collection: M.G.D. and C.N.R.; Resources: C.E.D.; Data analysis and interpretation: C.N.R.; Writing-original draft preparation: M.G.D., C.N.R. and C.E.D.; Writing-review & editing: M.G.D., C.N.R. and C.E.D.; Supervision: M.G.D.; Project administration: C.N.R.
REFERENCES
1. Kihara H., Sugawara S., Yokota J., Takafuji K., Fukazawa S., Tamada A., et al. Applications of three-dimensional printers in prosthetic dentistry. J Oral Sci [Internet]. 2021; 63 (3): 212-6. Available at: http://dx.doi.org/10.2334/josnusd.21-0072
2. Eaton K.A. The development of digital dentistry in the UK: An overview. Prim Dent J [Internet]. 2022; 11 (4): 94-8. Available at: http://dx.doi.org/10.1177/20501684221134198
3. Khanagar S.B., Al-Ehaideb A., Vishwanathaiah S., Maganur P.C., Patil S., Naik S., et al. Scope and performance of artificial intelligence technology in orthodontic diagnosis, treatment planning, and clinical decision-making - A systematic review. J Dent Sci [Internet]. 2021; 16 (1): 482-92. Available at: http://dx.doi.org/10.1016/j.jds.2020.05.022
4. Pandey R., Kamble R., Kanani H. Revolutionizing smiles: Advancing orthodontics through digital innovation. Cureus [Internet]. 2024; 16 (7): e64086. Available at: http://dx.doi.org/10.7759/cureus.64086
5. Tanna N.K., Almuzaini A., Mupparapu M. Imaging in Orthodontics. Dental Clinics of North America. 2021; 65.
6. Rischen R.J., Breuning K.H., Bronkhorst E.M., Kuijpers-Jagtman A.M. Records needed for orthodontic diagnosis and treatment planning: a systematic review. PLoS One [Internet]. 2013; 8 (11): e74186. Available at: http://dx.doi.org/10.1371/journal.pone.0074186
7. Nordblom N.F., Büttner M., Schwendicke F. Artificial intelligence in orthodontics: Critical review. J Dent Res [Internet]. 2024; 103 (6): 577-84. Available at: http://dx.doi.org/10.1177/00220345241235606
8. Kumari A., Nayak T.K., Pattanaik S. Digital model in orthodontics. Indian J Public Health Res Dev [Internet]. 2019; 10 (11): 1116. Available at: http://dx.doi.org/10.5958/0976-5506.2019.03659.3
9. Pachêco-Pereira C., De Luca Canto G., Major P.W., Flores-Mir C. Variation of orthodontic treatment decision-making based on dental model type: A systematic review. Angle Orthod [Internet]. 2015; 85 (3): 501-9. Available at: http://dx.doi.org/10.2319/051214-343.1
10. Schierz O., Hirsch C., Krey K.-F., Ganss C., Kämmerer P.W., Schlenz M.A. Digital dentistry and its impact on oral health-related quality of life. J Evid Based Dent Pract [Internet]. 2024; 24 (1S): 101946. Available at: http://dx.doi.org/10.1016/j.jebdp.2023.101946
11. Murugesan A., Sivakumar A. Comparison of accuracy of mesiodistal tooth measurements made in conventional study models and digital models obtained from intraoral scan and desktop scan of study models. J Orthod [Internet]. 2020; 47 (2): 149-55. Available at: http://dx.doi.org/10.1177/1465312520910755
12. Liczmanski K., Stamm T., Sauerland C., Blanck-Lubarsch M. Accuracy of intraoral scans in the mixed dentition: a prospective non-randomized comparative clinical trial. Head Face Med [Internet]. 2020; 16 (1): 11. Available at: http://dx.doi.org/10.1186/s13005-020-00222-6
13. Gavounelis N.A., Gogola C.-M.C., Halazonetis D.J. The effect of scanning strategy on intraoral scanner’s accuracy. Dent J [Internet]. 2022; 10 (7): 123. Available at: http://dx.doi.org/10.3390/dj10070123
14. Hou D., Capote R., Bayirli B., Chan D.C.N., Huang G. The effect of digital diagnostic setups on orthodontic treatment planning. Am J Orthod Dentofacial Orthop [Internet]. 2020; 157 (4): 542-9. Available at: http://dx.doi.org/10.1016/j.ajodo.2019.09.008
15. Golez A., Vrcon C., Ovsenik M. Jaw morphology and factors associated with upper impacted canines: Case-controlled trial. Appl Sci (Basel) [Internet]. 2024; 14 (17): 7700. Available at: http://dx.doi.org/10.3390/app14177700
16. Gracea R.S., Winderickx N., Vanheers M., Hendrickx J., Preda F., Shujaat S., et al. Artificial intelligence for orthodontic diagnosis and treatment planning: A scoping review. J Dent [Internet]. 2025; 152 (105442): 105442. Available at: http://dx.doi.org/10.1016/j.jdent.2024.105442
17. Balashova M., Khabadze Z., Popaduk V., Kulikova A., Bakaev Y., Abdulkerimova S. Artificial intelligence application in assessment of upper airway on cone-beam computed tomography scans. Ebsco.com. 2023; 14 (6).
18. Mohammed H., Daniel B.K., Farella M. Smile analysis in dentistry and orthodontics-a review. J R Soc N Z [Internet]. 2025; 55 (1): 192-205. Available at: http://dx.doi.org/10.1080/03036758.2024.2316226
19. Chung E.-J., Yang B.-E., Park I.-Y., Yi S., On S.-W., Kim Y.-H., et al. Effectiveness of cone-beam computed tomography-generated cephalograms using artificial intelligence cephalometric analysis. Sci Rep [Internet]. 2022; 12 (1): 20585. Available at: http://dx.doi.org/10.1038/s41598-022-25215-0
20. Charavet C., Bernard J.-C., Gaillard C., Le Gall M. Benefits of Digital Smile Design (DSD) in the conception of a complex orthodontic treatment plan: A case report-proof of concept. Int Orthod [Internet]. 2019; 17 (3): 573-9. Available at: http://dx.doi.org/10.1016/j.ortho.2019.06.019
21. Adel S.M., Bichu Y.M., Pandian S.M., Sabouni W., Shah C., Vaiid N. Clinical audit of an artificial intelligence (AI) empowered smile simulation system: a prospective clinical trial. Sci Rep [Internet]. 2024; 14 (1): 19385. Available at: http://dx.doi.org/10.1038/s41598-024-69314-6
22. De Leotard A., Le Norcy E. Comparison of dental movements in digital setups created by orthodontists and “3shape design service®” engineers: A cross-sectional study. Int Orthod [Internet]. 2024; 22 (4): 100919. Available at: http://dx.doi.org/10.1016/j.ortho.2024.100919
 Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.
Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.