Odovtos-International Journal of Dental Sciences (Odovtos-Int. J. Dent. Sc.), Online First, 2025. ISSN: 2215-3411
https://doi.org/10.15517/bfajm739

https://revistas.ucr.ac.cr/index.php/Odontos
BASIC RESEARCH:
Evaluating Mandibular Condyle Position Changes After Orthognathic Surgery:
A Systematic Review and Meta-Analysis
Evaluación de los cambios en la posición del cóndilo mandibular después de cirugía ortognática:
una revisión sistemática y metaanálisis
Ali Sharifi¹ https://orcid.org/0009-0001-5254-8604
Mehran Rahbar¹ https://orcid.org/0009-0000-6541-2952
Mojtaba Sheykhian¹ https://orcid.org/0009-0000-6541-8369
Javad Hayati Garjan¹ https://orcid.org/0009-0005-6947-5535
¹Department of Oral and Maxillofacia Surgery, Faculty of Dentistry, Tabriz University of Medical Science, Tabriz, Iran.
Correspondence to: Ali Sharifi - alisharifi19951374@gmail.com
Received: 1-IV-2025 Accepted: 24-VII-2025
ABSTRACT: Present research aims to evaluate mandibular condyle position changes after bilateral sagittal split osteotomy and bimaxillary orthognathic surgery. Relevant keywords were searched in the international databases Cochrane, Embase, and MEDLINE (PubMed and Ovid) up to January 2025. The Newcastle-Ottawa Scale used to determine the quality of the studies. Mean change of condylar values was used as an effect size with random-effects model and REML methods of 95% confidence intervals (CI). Meta-analysis performed using Stata (as of version 17). The mean change of left condylar position pre- and postoperative values of BSSO was -0.28º (ES -0.28º 95% CI; -1.59º, 1.03º; p<0.05). Non-significant mean values of condylar position pre- and postoperative of BSSO and bimaxillary orthognathic surgery in left sagittal plane was observed (p>0.05). The mandibular condyle position after surgery is influenced to some extent by orthognathic surgery.
KEYWORDS: Orthognathic surgery; Mandibular condyle; Orthognathic surgical procedures.
RESUMEN: La presente investigación tiene como objetivo evaluar los cambios en la posición del cóndilo mandibular tras la osteotomía sagital bilateral (BSSO) y la cirugía ortognática bimaxilar. Se realizó una búsqueda de palabras clave relevantes en las bases de datos internacionales Cochrane, Embase y MEDLINE (PubMed y Ovid) hasta enero de 2025. La calidad de los estudios se determinó mediante la escala Newcastle-Ottawa. El cambio promedio de los valores condilares se utilizó como medida de efecto, aplicando un modelo de efectos aleatorios y métodos REML con intervalos de confianza (IC) del 95%. El metaanálisis se llevó a cabo utilizando Stata (versión 17). El cambio promedio en la posición condilar izquierda entre los valores pre y postoperatorios de BSSO fue de -0.28º (ES -0.28º; IC 95%: -1.59º, 1.03º; p<0.05). Se observaron valores promedio no significativos en la posición condilar pre y postoperatoria de BSSO y de cirugía ortognática bimaxilar en el plano sagital izquierdo (p>0.05). Los hallazgos sugieren que la posición del cóndilo mandibular después de la cirugía se ve influida, en cierta medida, por la intervención ortognática.
PALABRAS CLAVE: Cirugía ortognática; Cóndilo mandibular; Procedimientos quirúrgicos ortognáticos.
Introduction
Correct maxillofacial occlusal inconsistencies and abnormalities can be corrected with different orthognathic surgery methods (1). Mandibular and/or maxillary osteotomy are orthognathic surgery methods (2). Airway obstruction, facial harmony, and temporomandibular joint (TMJ) function should be carefully evaluated in preoperative planning (3). One of the most commonly used techniques, introduced by Obwegeser and Trauner, is bilateral sagittal split osteotomy (BSSO) (4). In BSSO, the lower jaw is separated from the face and placed in position (5). The medical technique for internally set and stabilization of broken bones is internal fixation (IF), which generally uses bicortical or monocortical screws and miniplates (6). TMJ function, long-term skeletal stability, and favorable postoperative outcomes all depend on proper condylar seating. Malocclusion can result from central or peripheral condylar sagging, either during the recovery process after the perioperative maxillomandibular fixation (MMF) is removed. In addition, condylar resorption and skeletal relapse may occur (6).
The condyle must not be rotated or displaced during mandibular osteosynthesis (7). With proper surgical technique, condylar remodeling should be minimal. There is an ongoing debate about the choice between semi-rigid internal fixation and rigid internal fixation (RIF). To facilitate postoperative skeletal stability, segmental displacement must be avoided by removing all bony interference and leaving the necessary gaps between segments (8). Condylar position and postoperative TMJ function can be influenced by all mandibular osteosynthesis techniques used in orthognathic surgery. Temporomandibular joint dysfunction can result from incorrect postoperative condylar position, future condylar resorption, and disc displacement (9-11). Due to the importance of the issue, present research aims to evaluate mandibular condyle position changes after BSSO and bimaxillary orthognathic surgery.
Method
Search strategy and Information sources
To determine the purpose of the study, relevant keywords were searched in the international databases Cochrane, Embase, and MEDLINE (PubMed and Ovid) up to January 2025. Google Scholar, CENTRAL (Cochrane Central Register of Controlled Trials), WOS (Web of Science), EBSCO, ISI, Elsevier, and the Scopus Wiley Online Library were also consulted. The current study is based on the 27-point checklist PRISMA 2020 (12).
The search strategy used in MEDLINE (via PubMed):
(((((((("Orthognathic Surgery" [Mesh] OR "Orthognathic Surgical Procedures" [Mesh]) OR "Orthognathic Surgery/methods" [Mesh]) OR "Surgery, Oral" [Mesh]) AND "Mandibular Condyle" [Mesh]) OR ("Mandibular Condyle/diagnostic imaging" [Mesh] OR "Mandibular Condyle/injuries" [Mesh] OR "Mandibular Condyle/surgery" [Mesh])) AND "Mandible" [Mesh]) AND "Jaw" [Mesh]) AND "Postoperative Period" [Mesh]) AND "Preoperative Period" [Mesh].
The search strategy used in Cochrane:
"Orthognathic Surgery" OR "bilateral sagittal split osteotomy" OR "bimaxillary surgery" AND "Condylar position" OR "mandibular condyle" OR "condylar position changes" AND "Preoperative" AND "postoperative" AND "axial planes" OR "sagittal planes".
The search strategy used in Embase:
(Orthognathic Surgery) OR (bilateral sagittal split osteotomy) OR (bimaxillary surgery): ab,ti,kw
Mandibular condyle: ab,ti,kw
(Condylar position) OR (condylar position changes): ab,ti,kw
Selection criteria
Only studies published in English were considered. The PICO strategy was used to answer the questions in the present study. Population (P): Patients undergoing BSSO and bimaxillary; Intervention (I): BSSO or bimaxillary; comparison (C): pre- and postoperative; Outcome (O): condylar position changes. studies have been conducted in a review, laboratory and animal form; books; qualitative studies; Studies with incomplete data and case report studies were excluded from the study.
The process of selection and
data collection
Two blind and independent researchers reviewed the data of the selected studies and the third researcher summarized. The data was collected using a pre-designed form by the research team that includes sections such as the name of the first author of the study, year of publication, study design, number of patients, gender, mean age, malocclusion type, orthognathic surgery and radiographic evaluation.
Statistical heterogeneity
Chi-square test (χ2) and I2 to determine heterogeneity between studies. The value of I2 checked in four levels (low heterogeneity: ≤25%; moderate: 25%-50%; substantial: 50%-75%; considerable: ≥ 75%.
Methodological quality
The Newcastle-Ottawa Scale (NOS) was used to determine the quality of the studies. This scale examines the risk of bias in three areas: study group selection, group comparability, and outcome determination. For each study, a total score was created by adding up the ratings assigned to each criterion. Based on NOS scores, studies were classified into low (7-9), medium (4-6), or high (0-3) risk of bias studies.
Data analysis
Mean change of condylar values was used as an effect size with random-effects model and REML methods of 95% confidence intervals (CI). Meta-analysis performed using Stata (as of version 17). Statistical significance was considered less than 0.05.
Results
Description of studies
A total of 219 articles were found in international databases during the initial search using related keywords. Two blind, independent researchers reviewed the articles and eliminated any articles that were duplicate or unrelated to the study topic. Abstracts of 143 studies were reviewed based on the inclusion criteria (109 articles were removed at this stage); the full texts of 34 articles were examined; only nine of these articles were included in the study because they were consistent with the objectives (Figure 1).
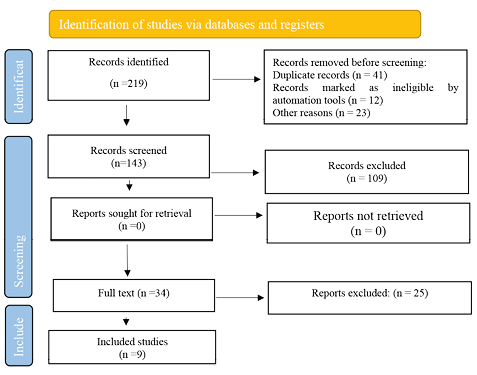
Figure 1. PRISMA 2020 Checklist.
Study characteristics
A total of 324 patients (192 female and 11 male; One study did not report the gender of the participants (13) ) with 25.30 mean age were included. Malocclusion III, II and I were reported in 194, 50 and 5 patients, respectively; Two studies did not report the type of malocclusion (14, 15). BSSO was performed in 154 patients (11, 13, 14, 16). Bimaxillary surgery was performed in 170 patients(11, 17) (15, 18-20). Five (11, 13, 14, 16, 19) and four studies (15, 17, 18, 20) examined CT scan and CBCT before and after surgery, respectively (Table 1).
Bias Assessments
As shown in Table 2, one study was rated as "fair" by NOS (13), and eight studies were of high quality.
Axial plane
The mean change of left condylar position pre- and postoperative values of BSSO was -0.28º (ES -0.28º 95% CI; -1.59º, 1.03º; p<0.05), a significant inward rotation of the left condyle after BSSO. I2 statistic was 0% (p=0.99) that showed low heterogeneity (Figure 2).
The mean change of left condylar position pre- and postoperative values of bimaxillary orthognathic surgery was –0.30º (ES -0.30º 95% CI; -1.35º, 0.76º; p<0.05), a significant inward rotation of the left condyle after bimaxillary orthognathic surgery. I2 statistic was 0% (p=1.00) that showed low heterogeneity (Figure 2).
According to test of group differences, left condylar position changes was similar between the bimaxillary and BSSO (p=0.99) (Figure 2).
No significant change was observed between mean change of right condylar position pre- and postoperative values of BSSO (ES 1.03º 95% CI; -0.36º, 2.43º; p>0.05) and bimaxillary orthognathic surgery (ES 0.28º 95% CI; -0.77º, 1.34º; p>0.05) (Figure 3). According to test of group differences, right condylar position changes were almost the same in both groups (p=40) (Figure 3).
The mean difference of left and right condylar position pre- and postoperative values of BSSO and bimaxillary orthognathic surgery was not statistically significant (p>0.05); No significant difference was observed between the groups (p=0.51, p=0.14) (Figure 4 and Figure 5).
Coronal plane
Non-significant mean values of condylar position pre- and postoperative of BSSO and bimaxillary orthognathic surgery in left sagittal plane was observed (p>0.05) (Figure 6).
Right condyle rotated outward postoperatively after BSSO (ES 0.23º 95% CI; -1.08º, 1.54º; p<0.05) and bimaxillary orthognathic surgery (ES 0.13º 95% CI; -1.01º, 1.27º; p<0.05). two groups were similar (p=0.91) (Figure 7).
Table 1. Characteristics of included studies.
|
Study Years |
Study design |
Number of patients |
Gender |
Mean age |
Malocclusion type (n) |
Orthognathic surgery |
Radiographic evaluation |
|
|
Female |
Male |
|||||||
|
Dvoranova et al., 2024 (11) |
ReS |
99 |
79 |
20 |
27.5 |
III malocclusion (57) II malocclusion |
BSSO (51) BOS (48 |
CT scans |
|
Buch et al., 2024 (17) |
ReS |
16 |
5 |
11 |
27 |
III malocclusion (7) II malocclusion (4) I malocclusion (5) |
BOS |
CBCT |
|
Küçükçakır et al., 2024 (18) |
ReS |
44 |
20 |
24 |
22.6 |
III malocclusion (44) |
BOS |
CBCT |
|
Kaur et al., 2022 (14) |
PoS |
37 |
18 |
19 |
22 |
NR |
BSSO |
CT scans |
|
Lee et al., 2022 (19) |
PoS |
11 |
7 |
4 |
21.1 |
III malocclusion |
BOS |
CT scans |
|
Park et al., 2022 (20) |
ReS |
23 |
14 |
9 |
22.5 |
III malocclusion |
BOS |
CBCT |
|
Shrestha et al., 2021 (13) |
ReS |
21 |
NR |
NR |
24 |
III malocclusion |
BSSO |
CT scans |
|
Hirjak et al., 2020 (16) |
ReS |
45 |
34 |
11 |
30 |
III malocclusion (31) II malocclusion (14) |
BSSO |
CT scans |
|
Claus et al., 2019 (15) |
ReS |
28 |
15 |
13 |
31.07 |
NR |
BOS |
CBCT |
ReS: retrospective study; PoS: prospective study; BSSO: bilateral sagittal split osteotomy; BOS: Bimaxillary orthognathic surgery; NR: not reported.
Table 2. Bias assessments of included studies according to NOS scale.
|
Study. Years |
Selection |
Comparability |
Outcomes |
Score |
|||||
|
A |
B |
C |
D |
E |
F |
G |
H |
||
|
Dvoranova et al., 2024 (11) |
★ |
★ |
★ |
★ |
☆★ |
★ |
★ |
★ |
8 |
|
Buch et al., 2024 (17) |
★ |
★ |
★ |
★ |
☆★ |
★ |
★ |
★ |
8 |
|
Küçükçakır et al., 2024 (18) |
★ |
★ |
★ |
★ |
☆☆ |
★ |
★ |
★ |
7 |
|
Kaur et al., 2022 (14) |
★ |
★ |
★ |
★ |
☆★ |
★ |
★ |
★ |
8 |
|
Lee et al., 2022 (19) |
★ |
★ |
★ |
★ |
☆★ |
★ |
★ |
★ |
8 |
|
Park et al., 2022 (20) |
★ |
★ |
★ |
★ |
☆★ |
★ |
★ |
★ |
8 |
|
Shrestha et al., 2021 (13) |
★ |
☆ |
☆ |
★ |
☆★ |
★ |
★ |
★ |
6 |
|
Hirjak et al., 2020 (16) |
★ |
★ |
★ |
★ |
☆★ |
★ |
★ |
★ |
8 |
|
Claus et al.,2019 (15) |
★ |
★ |
★ |
★ |
☆★ |
★ |
☆ |
★ |
7 |
A: Representativeness of the Exposed Cohort; B: Selection of the Non-Exposed Cohort; C: Ascertainment of Exposure; D: Demonstration That Outcome of Interest Was Not Present at Start of Study; E: Demonstration That Outcome of Interest Was Not Present at Start of Study; F: Assessment of Outcome; G: Follow-Up Long; H: Adequacy of Follow-Up of Cohorts.
Black stars (★) to signify that a study satisfactorily meets a specific criterion. White stars (☆) indicate that a criterion is not met.
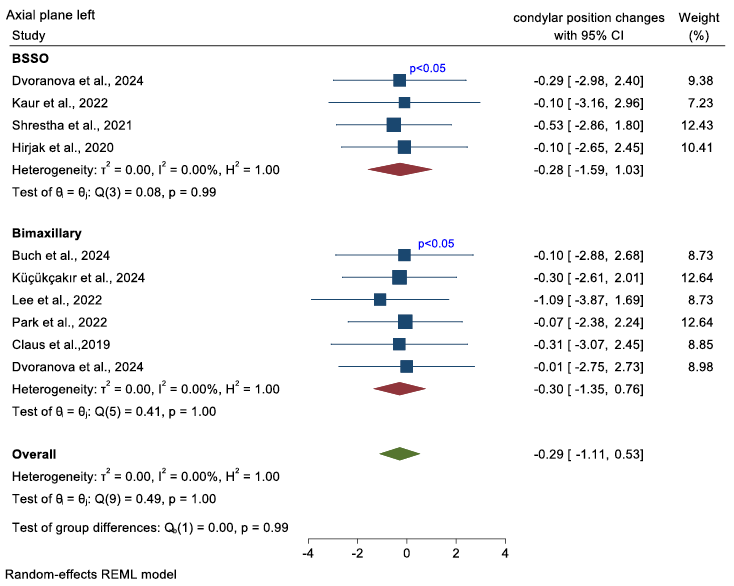
Figure 2. Forest plot showed mean change of left condylar position in axial plane pre- and postoperative values after orthognathic surgery.
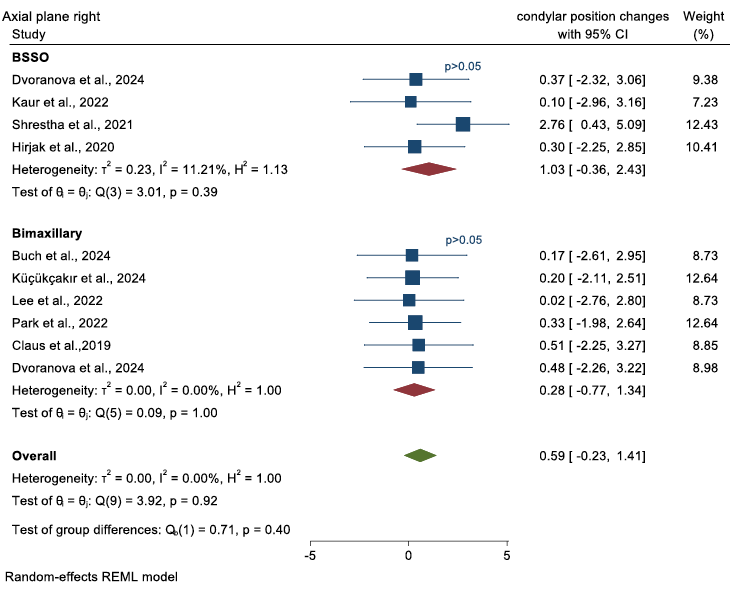
Figure 3. Forest plot showed mean change of right condylar position in axial plane pre- and postoperative values after orthognathic surgery.
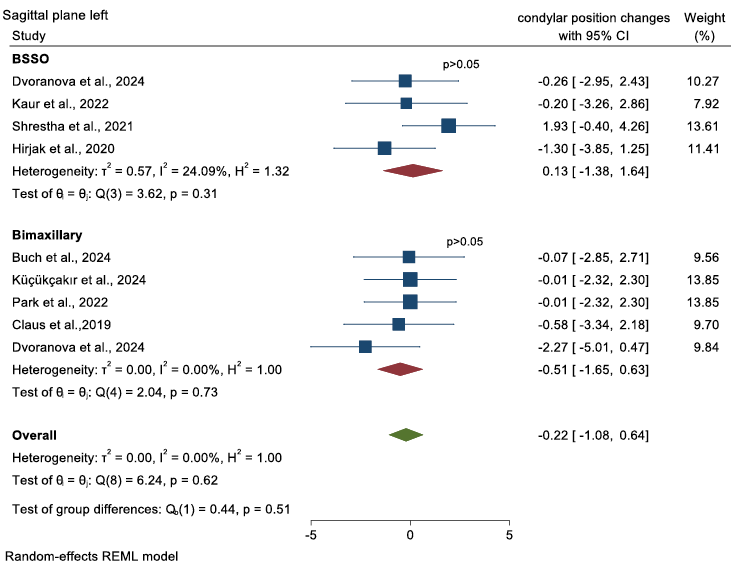
Figure 4. Forest plot showed mean change of left condylar position in sagittal plane pre- and postoperative values after orthognathic surgery.
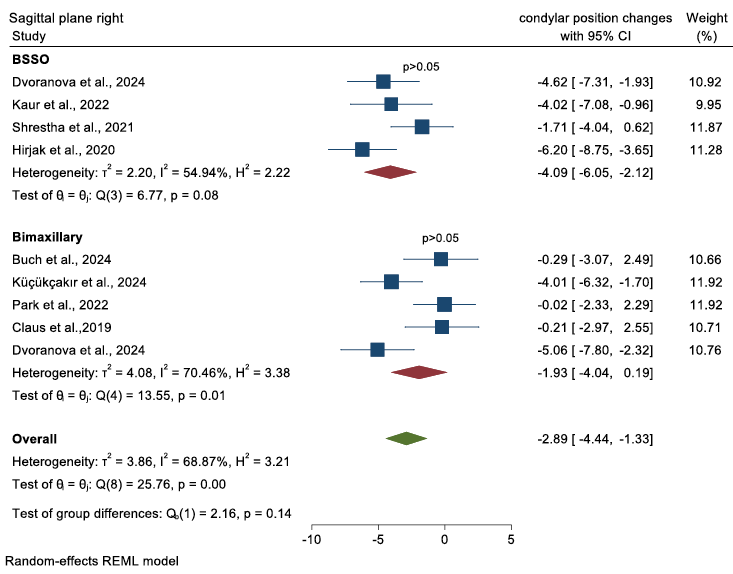
Figure 5. Forest plot showed mean change of right condylar position in sagittal plane pre- and postoperative values after orthognathic surgery.
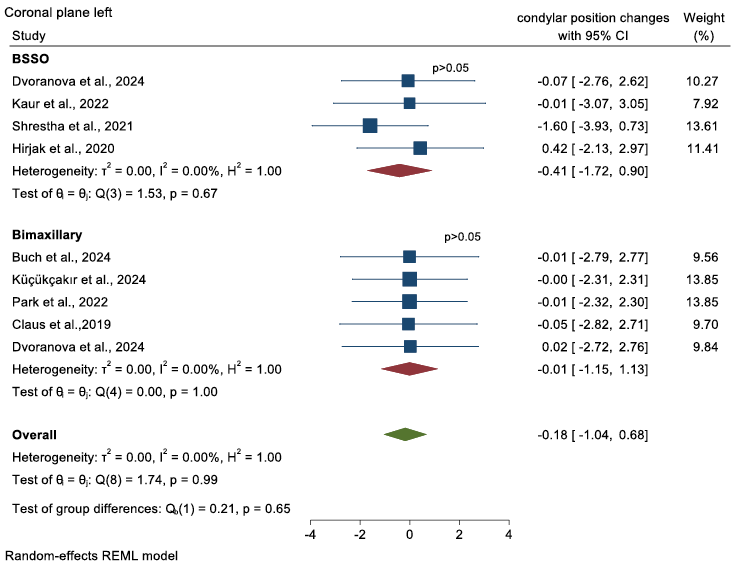
Figure 6. forest plot showed mean change of left condylar position in coronal plane pre- and postoperative values of orthognathic surgery.
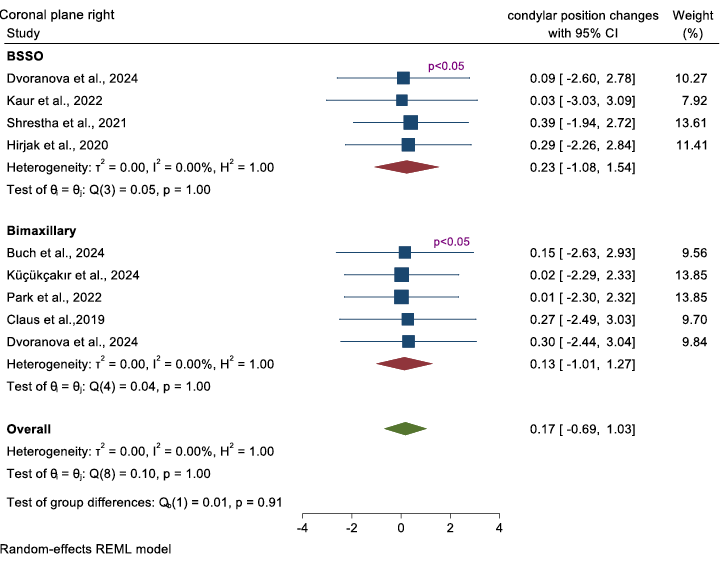
Figure 7. forest plot showed mean change of right condylar position in coronal plane pre- and postoperative values of orthognathic surgery.
Discussion
Condylar resorption, malocclusion, skeletal relapse, and TMJ dysfunction can all result from changes in condylar position after orthognathic surgery (21). Peripheral and central are the two main categories that Reyneke and Ferretti (2002) divided the various forms of condylar displacement and condylar sagging (22). Other factors affecting condylar position include the extent of segment movement, local anatomy, the presence of possible bony interference, and the experience of the surgeon performing the procedure. The degree of mandibular rotation, the extent of distal segment movement, and local anatomy all suggested that the shape of the mandible may be important, according to Harris et al. (1992)(23).
Following orthognathic surgery, condylar position may also be significantly influenced by the type of osteosynthesis (7). Notwithstanding the documented risk of condylar displacement and increased rates of skeletal relapse, some studies continue to advocate for bicortical screws (24). One miniplate with monocortical screws is preferred by some studies, while two miniplates are used by others studies (8, 25). Using bicortical screws to fix BSSO did not significantly alter condylar position or function, according to studies (26, 27). Studies reported once orthognathic surgery is completed, mild condylar remodeling is typical(28-30).
In the present study, observed that significant changes in pre-and postoperative values in left and right condyle in the axial plane, also right condyle rotated outward postoperatively in the coronal plane. Jung et al. (2017), who evaluated CT images with a condylar positioning plate, found that the angle of the left condylar axis was significantly different, while there were no noticeable differences on the right side(31). Choi et al. (2018) observed an increase in α-angle after surgery, which returned to preoperative levels six months later(32). Kim et al. (2010), revealed that the angle of the mandibular condyle increased by 2.23° on the right side and 2.18° on the left side, resulting in internal rotation (33).
A meta-analysis study was not found that could compare the results, however, in a review study it was shown that increased risk of Condylar resorption after orthognathic surgery was associated with mandibular advancement superior than 10 mm, reverse condylar repositioning, and counterclockwise rotation of the mandible (21). Barretto et al., 2022 in a systematic review evaluate methods of mandibular condyle position and rotation center used for orthognathic surgery planning and showed axis of rotation for orthognathic surgery planning must be fixed, permit individualization for each condyle and be reproducible.
Conclusion
According to the present meta-analysis, the mandibular condyle position after surgery is influenced to some extent by orthognathic surgery; more care should be taken when rotating the condyle in the transverse axis. Due to the small number of selected study samples and the difference in evaluation methods, more studies are needed in terms of similar investigated parameters, long follow-up period, and higher sample size.
Conflict of Interests: Authors declare that there is no conflict of interests.
Ethical Approval: Not Applicable.
Informed Consent: Not Applicable.
Funding: The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author contribution statement: Conceptualization and design:, A.S., M.R., M.S. and J.H.G; Literature Review, A.S., M.R., M.S. and J.H.G; Methodology and Validation, A.S., M.R., M.S. and J.H.G; Formal Analysis, A.S., and M.R.; Investigation and Data Collection, A.S., and M.R.; Resources, A.S., and M.R.; Data Analysis and Interpretation, A.S., M.R., M.S. and J.H.G; Writing-Original Draft Preparation, A.S.; Writing-Review & Editing, A.S.; Supervision, A.S., and M.R.; Project Administration, A.S.; Funding Acquisition, A.S. and M.R.”
References
1. Seo H.J., Choi Y.-K. Current trends in orthognathic surgery. Archives of Craniofacial Surgery. 2021; 22 (6): 287.
2. Bahmanyar S., Namin A.W., Weiss II R.O., Vincent A.G., Read-Fuller A.M., Reddy L.V. Orthognathic surgery of the mandible. Facial Plastic Surgery. 2021; 37 (06): 716-21.
3. Reyneke J.P., Ferretti C. Diagnosis and planning in orthognathic surgery. Oral and maxillofacial surgery for the clinician. 2021:1 437-62.
4. Prasad V., Kumar S., Pradhan H., Siddiqui R., Ali I. Bilateral sagittal split osteotomy a versatile approach for correction of facial deformity: a review literature. National Journal of Maxillofacial Surgery. 2021; 12 (1): 8-12.
5. Heller U., Vacher C., Loncle T. Evaluation of the lower face enlargement following mandibular osteotomy: Bilateral sagittal split osteotomy (BSSO) vs supra basilar sagittal Split Osteotomy (SBSSO). Journal of Stomatology, Oral and Maxillofacial Surgery. 2023; 124 (5): 101488.
6. İnan Ö.M., Karaca İ., Dolanmaz D. Fixation Methods Used in Sagittal Split Ramus Osteotomy. EurAsian Journal of Oral and Maxillofacial Surgery. 3 (1): 43-51.
7. Pachnicz D., Ramos A. Mandibular condyle displacements after orthognathic surgery-an overview of quantitative studies. Quantitative Imaging in Medicine and Surgery. 2021; 11 (4): 1628.
8. Arnett G.W., Gunson M.J., editors. Risk factors in the initiation of condylar resorption. Seminars in Orthodontics; 2013: Elsevier.
9. Abrahamsson C., Henrikson T., Nilner M., Sunzel B., Bondemark L., Ekberg E. TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. International journal of oral and maxillofacial surgery. 2013; 42 (6): 752-8.
10. Kretschmer W., Baciuţ G., Baciuţ M., Sader R. Effect of bimaxillary orthognathic surgery on dysfunction of the temporomandibular joint: a retrospective study of 500 consecutive cases. British Journal of Oral and Maxillofacial Surgery. 2019; 57 (8): 734-9.
11. Dvoranova B., Vavro M., Czako L., Hirjak D. Does orthognathic surgery affect mandibular condyle position? A retrospective study. Oral and maxillofacial surgery. 2024; 28 (2): 639-43.
12. Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. bmj. 2021; 372.
13. Shrestha A., Song S.H., Aung H.N., Sangwatanakul J., Zhou N. Three-dimensional cephalometric analysis: the changes in condylar position pre-and post-orthognathic surgery with skeletal class III malocclusion. Journal of Craniofacial Surgery. 2021; 32 (2): 546-51.
14. Kaur A., Rattan V., Rai S., Singh S.P., Kalra P., Sharma S. Changes in condylar position after orthognathic surgery and its correlation with temporomandibular symptoms (TMD)-a prospective study. Journal of Cranio-Maxillofacial Surgery. 2022; 50 (12): 915-22.
15. Claus J., Koerich L., Weissheimer A., Almeida M., de Oliveira R.B. Assessment of condylar changes after orthognathic surgery using computed tomography regional superimposition. International journal of oral and maxillofacial surgery. 2019;48 (9): 1201-8.
16. J.P. R. Condylar position and mandibular function after bilateral sagittal split osteotomy. Bratislava Medical Journal/Bratislavské Lekárske Listy. 2020; 121 (6).
17. Buch F.O., Stokbro K. Accuracy and stability of the condyle position after orthognathic surgery: A retrospective study. Journal of Cranio-Maxillofacial Surgery. 2024; 52 (2): 240-5.
18. Küçükçakır O., Ersan N., Arslan Y.Z., Cansız E. Evaluation of mandibular condyle position in Class III patients after bimaxillary orthognathic surgery: A cone-beam computed tomography study. Korean Journal of Orthodontics. 2024; 54 (4): 247-56.
19. Lee Y.-C., Sohn H.-B., Park Y.-W., Oh J.-H. Evaluation of postoperative changes in condylar positions after orthognathic surgery using balanced orthognathic surgery system. Maxillofacial Plastic and Reconstructive Surgery. 2022; 44 (1): 11.
20. Park S.Y., Choi Y.-K., Lee S.H., Kang H.-J., Kim S.-S., Kim S.-H., et al. Long-term condylar remodelling after bimaxillary orthognathic surgery in skeletal Class III patients. British Journal of Oral and Maxillofacial Surgery. 2022;60(8):1056-61.
21. Catherine Z, Breton P, Bouletreau P. Condylar resorption after orthognathic surgery: A systematic review. Revue de Stomatologie, de Chirurgie Maxillo-faciale et de Chirurgie Orale. 2016; 117 (1): 3-10.
22. Reyneke J.P., Ferretti C. Intraoperative diagnosis of condylar sag after bilateral sagittal split ramus osteotomy. British Journal of Oral and Maxillofacial Surgery. 2002; 40 (4): 285-92.
23. Harris M.D., Van Sickels J.R., Alder M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. Journal of oral and maxillofacial surgery. 1999; 57 (6): 650-4.
24. Ochs M.W. Bicortical screw stabilization of sagittal split osteotomies. Journal of oral and maxillofacial surgery. 2003; 61 (12): 1477-84.
25. Joss C.U., Vassalli I.M. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. Journal of oral and maxillofacial surgery. 2009; 67 (2): 301-13.
26. Reyneke J., Hirjak D., Dvoranova B. Condylar position and mandibular function after bilateral sagittal split osteotomy. 2020.
27. Hirjak D., Beno M., Kupcova I., Branislav G. The position of the condyles and functional results after bilateral sagittal split osteotomy. International Journal of Oral and Maxillofacial Surgery. 2017; 46: 159.
28. Gallagher A.L., de Oliveira Ruellas A.C., Benavides E., Soki F.N., Aronovich S., Magraw C.B.L., et al. Mandibular condylar remodeling characteristics after simultaneous condylectomy and orthognathic surgery. American Journal of Orthodontics and Dentofacial Orthopedics. 2021; 160 (5): 705-17.
29. Hsu L.-F., Liu Y.-J., Kok S.-H., Chen Y.-J., Chen Y.-J., Chen M.-H., et al. Differences of condylar changes after orthognathic surgery among Class II and Class III patients. Journal of the Formosan Medical Association. 2022; 121 (1): 98-107.
30. Al-Rezami K.F., Abotaleb B.M., Alkebsi K., Wang R., Al-Nasri A., Sakran K., et al. Long-term three-dimensional condylar remodeling during presurgical orthodontics and after orthognathic surgery of mandibular retrognathia with high mandibular plane angle. Clinical Oral Investigations. 2022; 26 (12): 7253-63.
31. Jung G.S., Kim T.K., Lee J.W., Yang J.D., Chung H.Y., Cho B.C., et al. The effect of a condylar repositioning plate on condylar position and relapse in two-jaw surgery. Archives of Plastic Surgery. 2017; 44 (01): 19-25.
32. Choi B.-J., Kim B.-S., Lim J.-M., Jung J., Lee J.-W., Ohe J.-Y. Positional change in mandibular condyle in facial asymmetric patients after orthognathic surgery: cone-beam computed tomography study. Maxillofacial Plastic and Reconstructive Surgery. 2018; 40: 1-8.
33. Kim Y.I., Jung Y.H., Cho B.H., Kim J.R., Kim S.S., Son W.S., et al. The assessment of the short-and long-term changes in the condylar position following sagittal split ramus osteotomy (SSRO) with rigid fixation. Journal of oral rehabilitation. 2010; 37 (4): 262-70.
 Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.
Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.