LITERATURE REVIEW:
Selection Criteria for Radiographic Images in Dentistry: A Comprehensive Review of Updated Standards
Criterios de indicación de imágenes radiográficas en Odontología: una revisión actualizada
Lucía Barba Ramírez DDS, MSc¹ http://orcid.org/0000-0003-1457-7209
Ana Cecilia Ruiz-Imbert DDS, MSc2 https://orcid.org/0000-0002-0700-6814
Deivi Cascante-Sequeira DDS, MSc, PhD3 https://orcid.org/0000-0002-5009-6632
¹MSc Oral and Maxillofacial Radiology, Specialist in Oral and Maxillofacial Radiology. Professor in the Department of Diagnostic and Surgical Sciences, Faculty of Dentistry, University of Costa Rica, San José, Costa Rica.
²MSc Stomatology, Specialist in Oral and Maxillofacial Radiology. Professor in the Department of Diagnostic and Surgical Sciences, Faculty of Dentistry, University of Costa Rica, San José, Costa Rica.
3MSc, PhD in Oral and Maxillofacial Radiology, MSc Oral and Maxillofacial Radiology. Professor in the Department of Diagnostic and Surgical Sciences, Faculty of Dentistry, University of Costa Rica, San José, Costa Rica.
Correspondence to: MSc Lucía Barba Ramírez - LUCIA.BARBARAMIREZ@ucr.ac.cr
Received: 24-II-2025 Accepted: 6-V-2025
ABSTRACT: Radiographic images play a crucial role in dentistry for diagnosis, treatment planning, and follow-up. However, due to the potential risks associated with ionizing radiation, such studies should only be conducted following a comprehensive patient history and clinical evaluation that justify their necessity. In the dentistry field, various radiographic techniques are available to acquire both intraoral and extraoral images, as well as two-dimensional and three-dimensional images. The selection of an imaging technique should be guided by its diagnostic efficacy, that is, how effectively it meets the patient's needs. Each imaging method possesses unique advantages and limitations, influenced by technical factors, and must be tailored to the specific diagnostic requirements of individual cases. This review aims to provide an evidence-based update on the criteria for choosing imaging techniques across the various areas of dental specialization.
KEYWORDS: Radiology; Diagnostic imaging; Panoramic radiography; Bitewing radiography; Cone-beam computed tomography; Radiation protection.
RESUMEN: Las imágenes radiográficas constituyen un examen complementario para el diagnóstico, plan de tratamiento y seguimiento en odontología. Debido a los potenciales efectos adversos biológicos de las radiaciones ionizantes, los estudios radiográficos deben indicarse luego de una adecuada anamnesis y evaluación clínica, solo cuando su uso sea justificado. Actualmente en odontología existen técnicas radiográficas que proveen imágenes intraorales y extraorales, bidimensionales y tridimensionales. Estas deben indicarse según la eficacia diagnóstica de cada técnica, es decir del rendimiento que cada técnica ofrezca en beneficio del paciente. Cada técnica de imagen presenta ventajas y limitaciones que dependen de factores técnicos y que deben adecuarse a la tarea diagnóstica, realizando un análisis individual de caso. La presente revisión constituye una actualización basada en evidencia, sobre los criterios de indicación de imágenes según las diferentes áreas de especialización en odontología.
PALABRAS CLAVE: Radiología; Diagnóstico por imagen; Radiografía panorámica; Radiografía interproximal; Tomografía computarizada de haz cónico; Protección radiológica.
Copyright (c) 2025 Lucía Barba Ramírez, Ana Cecilia Ruiz-Imbert, Deivi Cascante-Sequeira.

Odovtos -Int J Dent Sc endoses to CC-BY-NC-SA 4.0.
INTRODUCTION
The diagnostic process in dentistry involves conducting a patient anamnesis and thorough clinical examination to identify the patient’s diagnostic needs (1). Based on this information, the dentist decides whether complementary radiographic examinations are necessary. The interpretation of these examinations, along with the clinical evaluation, enables the clinician to establish a diagnosis, develop a treatment plan, assess the effectiveness of the treatment, and follow-up (2).
Conventional radiographic examinations provide two-dimensional images, which can include both intraoral and extraoral radiographs. In contrast, cone-beam computed tomography (CBCT) offers three-dimensional imaging, specifically designed for dental applications. It reveals the anatomical complexity of the maxillofacial bone structures, addressing the limitations of two-dimensional images, such as the overlap of structures, distortion, and magnification (2-4).
Both two-dimensional and three-dimensional radiographic dental examinations use low and very low doses of ionizing radiation, so the biological effects related to patient exposure are associated with sublethal damage to DNA, mainly radiation-induced cancer (5,6,7). These effects are called stochastic (5, 6) because of their random probability of occurring without a dose threshold (5). Therefore, there is no safe dose; even minimal doses of radiation carry the probability of inducing cancer (5, 6) and the probability increases as the received dose increases.
Given the inherent risk associated with exposure to ionizing radiation, the justification for requesting and performing a radiographic examination is essential. The potential benefits to the patient must outweigh any potential risks. Additionally, the chosen examination should be the most appropriate for the patient's clinical needs to ensure that the benefits surpass the risks involved (7).
The process of justifying a radiographic acquisition is a collaborative effort between the maxillofacial radiologist and the referring dentist. The specialized training of the maxillofacial radiologist in imaging and health technologies enables them to make evidence-based decisions (5,6). Before performing or requesting a radiographic examination, the clinician should review the patient’s history, clinical information, and any previous radiographic examinations. It is also essential for the clinician to ensure that the requested study is appropriate for addressing the clinical need.
The maxillofacial radiologist is responsible for determining whether the request is justified. If it is not, the radiologist should suggest an alternative examination. They must be aware of the available alternatives and choose the most suitable one based on the diagnostic efficacy of each examination, which refers to how well each exam serves the patient’s benefit (6,8). Generally, the examination with the highest efficacy is recommended, as it provides the greatest benefit to the patient (9).
The advantages of three-dimensional examinations suggest they could replace two-dimensional examinations. However, this substitution should only occur if the three-dimensional examination proves to be more effective than the two-dimensional option for the specific needs of the patient. Currently, there is limited evidence regarding the diagnostic efficacy of CBCT for various indications in dentistry (8,10-12). Additionally, many clinicians receive training solely from equipment manufacturers and suppliers. This training often focuses only on their specific equipment and may lack evidence supporting its effectiveness in diagnostics and, consequently, its benefits for patients (8).
Due to the variety of radiographic examinations, clinical guidelines recommend their use based on evidence and diagnostic effectiveness, ensuring informed and responsible decision-making (6, 8). These recommendations help clinicians select appropriate examinations and allow radiologists to suggest tailored options (13).
Routine X-rays for new patients are not supported by evidence (14), and they are unnecessary if there are no signs of disease or pathology since the last X-ray (1). Therefore, this review provides guidelines for prescribing radiographic examinations and serves as a consultation document for clinicians. Recommended imaging techniques are based on diagnostic efficacy and their respective advantages and disadvantages (15). These recommendations should be tailored to each patient’s specific needs.
MAIN CHARACTERISTICS OF IMAGE FORMATION BY X-RAY TECHNIQUES
Different X-ray techniques applied to the same anatomical region can produce images showing the same structures. However, the projection phenomena in two-dimensional images and the reconstruction processes in three-dimensional images affect the quality and performance of the images obtained. Therefore, it is crucial to understand the key aspects of image formation in the X-ray techniques used in dentistry. This knowledge will help select the technique that provides the most comprehensive information based on diagnostic needs.
Two-dimensional images
Intraoral radiographic techniques
Intraoral radiographic techniques consist, mainly, of periapical and interproximal or bitewing radiographs. Periapical radiographs are useful for observing the entire tooth, from the apex to the crown, as well as the alveolar bone and the alveolar cortex. These radiographs can be obtained using either parallel or bisecting technique. When using parallel technique, periapical radiographs provide an accurate evaluation of the proximal coronal region. However, since the central X-ray beam does not strike this area perpendicularly, the effectiveness of this technique for evaluating enamel on the proximal surfaces and the dentin-enamel junction at the occlusal level is diminished.
Bitewing radiographs are useful for examining dental crowns, roots, and the supporting structures up to the middle third of the root. This technique enables a more accurate assessment of the interproximal surfaces and the distance between the cementoenamel junction and the crestal bone, thanks to the perpendicular angle of the X-ray beam directed at the dental crowns and alveolar crests. It allows for the detection of interproximal and secondary carious lesions, as well as the assessment of restorations. Additionally, it can reveal some occlusal carious lesions.
Both techniques provide high spatial resolution and contrast and can be performed in a dental office at a relatively low cost (14-16).
To achieve optimal performance with intraoral radiographic techniques, it is preferable to use image receptor-holders. These devices help maintain the parallelism between the longitudinal axis of the teeth and the image receptor, resulting in less distortion of structures in the images. Additionally, they enhance the reproducibility of the technique, which is essential for monitoring changes in structures over time. This also reduces the likelihood of retakes due to technical errors, ultimately leading to a lower radiation dose for patients (14,17).
In contrast, the bisecting-angle and adhesive techniques are less advisable. The bisecting-angle technique tends to produce more distortion errors, such as shortening and elongation, as well as issues with the centralization of the localizing cylinder. The adhesive bitewing technique complicates both vertical and horizontal angulation of the image receptor, often leading to increased overlap of proximal surfaces and excessive vertical angulation, which can impair diagnostic accuracy.
Extraoral radiographic techniques
The most common extraoral radiographic techniques in dentistry are panoramic radiography and lateral cephalometric teleradiography.
Panoramic radiography provides an overall view of the teeth, alveolar bone, and surrounding structures in the maxillofacial area. However, it has lower spatial resolution compared to periapical radiographs. In addition to the general limitations of two-dimensional imaging -such as overlapping structures, distortion, and magnification-panoramic radiography has a particular drawback: vertical distortion (16). This occurs because of the negative angulation of the X-ray beam during the imaging process, which affects the vertical relationships of the structures in the image and can obscure lesions on the crowns of the teeth. Along with horizontal distortion, positioning errors and artifacts further compromise the reliability of structural measurements (16).
While panoramic radiography has specific applications that are discussed in this article, it is crucial to note that using it routinely for evaluating new patients or at regular intervals is not justified.
Lateral cephalometric or profile teleradiography is a technique that allows for the visualization of the bones of the face and skull, as well as the profile of facial soft tissue. This standardized method is particularly useful for patients with skeletal discrepancies, as it helps evaluate the skeletal pattern (17).
Three-dimensional images
Cone Beam Computed Tomography (CBCT)
In CBCT, the X-ray tube produces a cone- or pyramid-shaped beam, generating three-dimensional images of the dentoalveolar or maxillofacial region. This technique addresses the limitations of two-dimensional images, although it has a variable spatial resolution compared to periapical radiographs (18).
The size of the tomographic volume is known as the field of view or FOV, which is measured in diameter and height and varies from small, to medium, or large, depending on each equipment. The resolution of CBCT examinations is influenced by several factors, one of which is the size of the voxel, the smallest unit of the tomographic image. Smaller voxel sizes lead to higher-resolution images. Additionally, the acquisition parameters, such as tube voltage and current, can be adjusted based on the patient's characteristics and the specific diagnostic requirements of the image (3). Therefore, a CBCT study should be customized for each individual case.
CBCT has specific indications that will be discussed later in this article. However, current evidence does not support its use for certain diagnoses because of the artifacts inherent to the technique. These artifacts can reduce diagnostic quality and complicate the evaluation of the coronal area of the teeth.
Criteria for the recommendations in this article
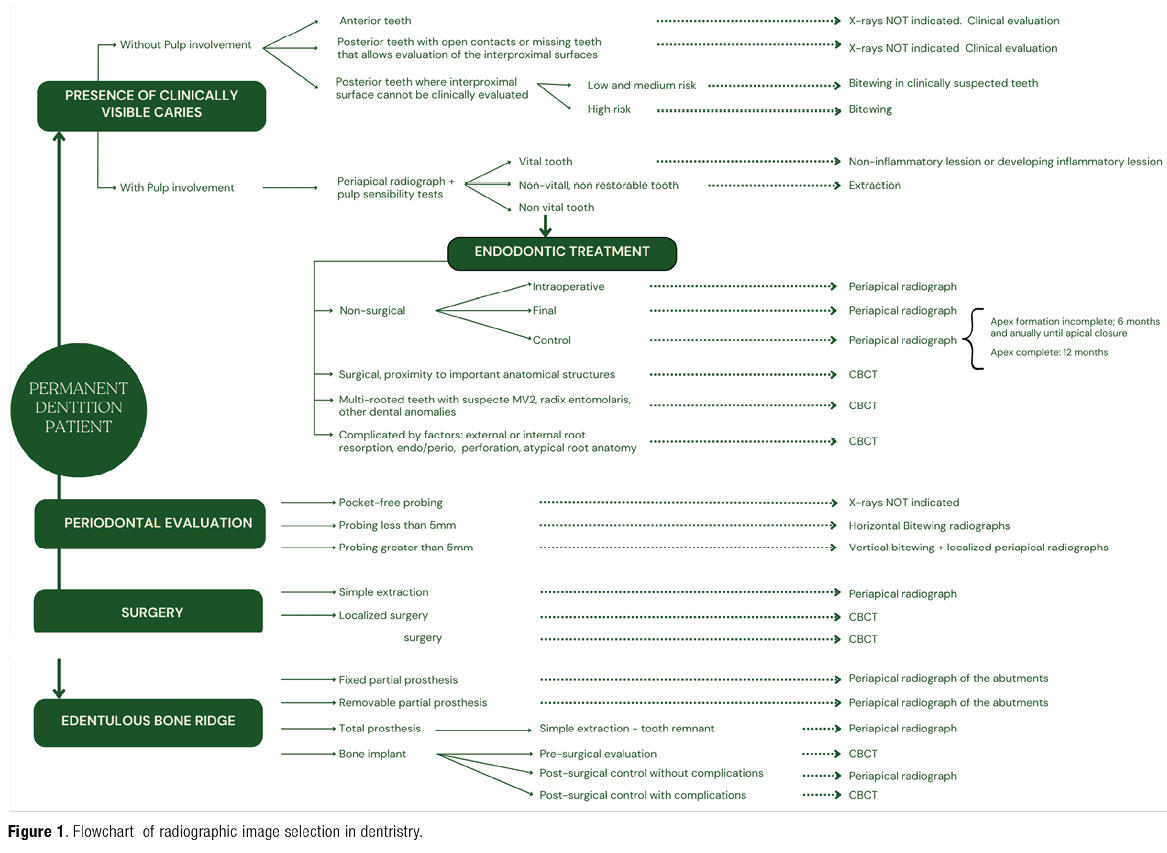
This article aims to justify the use of radiographic images based on specific needs. However, it's important to remember that the diagnostic approach should be comprehensive. After conducting a clinical examination, any necessary radiographs should only be defined if the required information cannot be obtained through clinical assessment. Once the radiographs are obtained, they should be thoroughly analyzed. Figure 1 presents a flowchart outlining the process for selecting radiographic images in dentistry.
The patient's record should include the clinical examination, symptoms and signs, the reason for the radiographic examination, the technique used, the date and number of radiographs taken, and the written radiological interpretation. Relevant information for specific needs should also be documented. Diagnostic errors occur when an imaging study is not thoroughly assessed, when findings are not reported, or are reported inaccurately (19, 20).
Diagnostic errors can lead to adverse outcomes for both patient and clinician, such as late diagnosis of serious diseases, unnecessary or harmful treatments, patient mortality (21-23), malpractice lawsuits, and damage to the clinician's reputation (24). Factors associated with these errors include a lack of clinical history, nondiagnostic radiographic images obtained with poor technique, poor knowledge update on the part of the interpreter, observation and lighting conditions (20,25).
The dentist must provide the maxillofacial radiologist with the patient's complete clinical history and be prepared to supply previous images or additional information if required for interpreting the images (13, 15, 20). When the dentist takes and interprets the images, he or she is responsible for the entire process, which must be documented in the patient's record.
1. Radiographic diagnosis of caries lesions
The request for radiographs to diagnose caries is based on evaluating caries risk. This evaluation also determines the interval for taking radiographs, which is personalized for each patient.
The date of the risk assessment, the risk level (low, moderate, high), and the date of the next assessment must be documented in the patient´s record (26). The intervals between subsequent radiographic examinations must be reassessed periodically, along with the evaluation of caries risk (15).
The use of bitewing radiographs with adhesive bitewings or periapical radiographs is not recommended due to previously mentioned limitations. Panoramic radiographs and CBCT are likewise not indicated (6, 15) (Table 1).
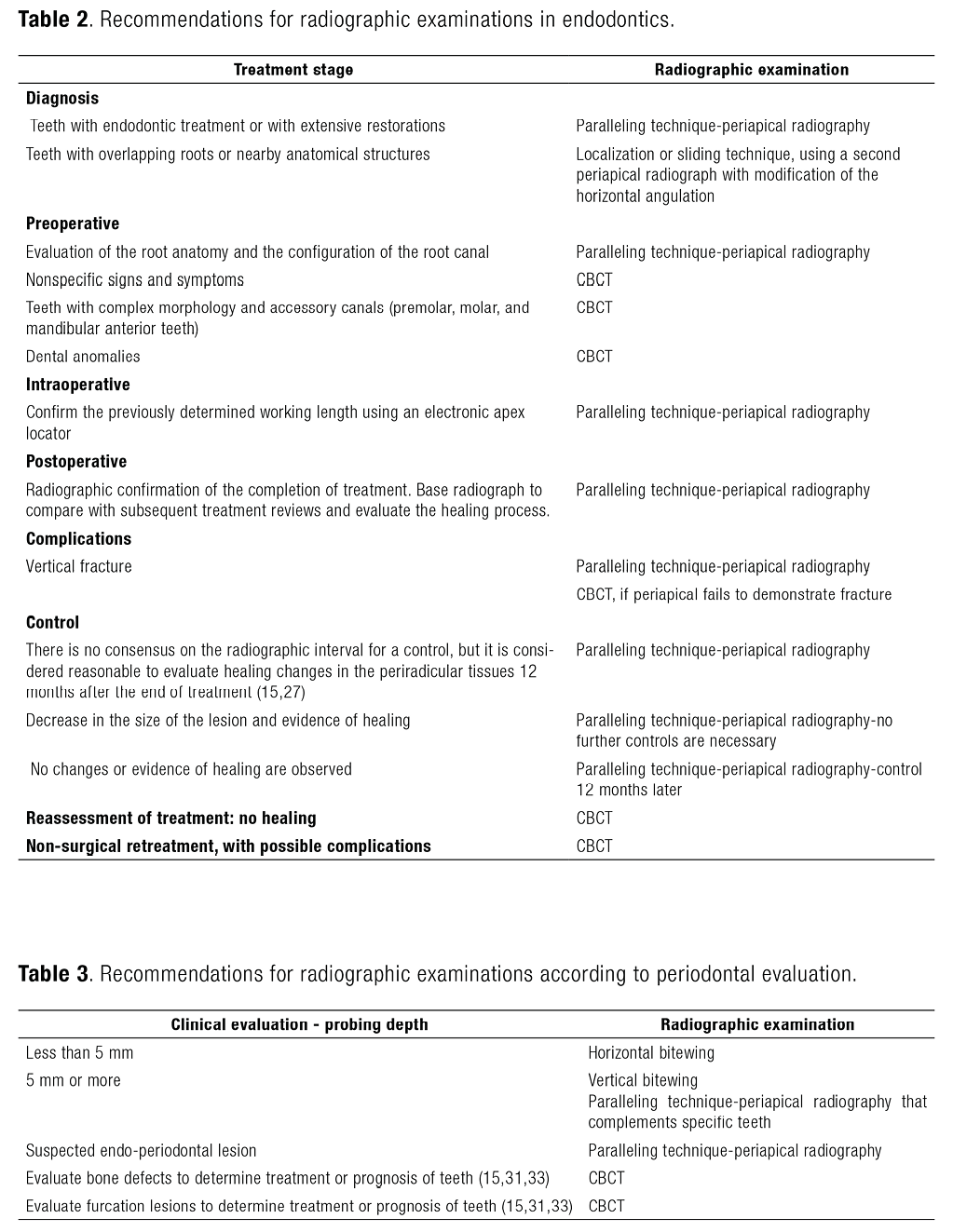
2. Diagnosis in endodontics
In endodontics, it is essential to use diagnostic tests such as palpation, mobility, percussion, periodontal evaluation, occlusal examination, and sensitivity (27).
The sensitivity tests for the diagnostic stage (27), the preoperative evaluation, the working length, the assessment of the final treatment, the presence of material extrusion, the type of restorative material, among others, must be recorded in the patient´s record (15, 27).
Paralleling technique is the recommended technique for evaluating teeth in endodontics. The bisecting-angle technique and panoramic radiography are not recommended for the reasons previously described regarding posible vertical distortion in the obtained images (28). Routine use of CBCT is not indicated since its use has been found to lead to overdiagnosis and overtreatment (29, 30). Nevertheless, there are specific cases in which CBCT must be used (Table 2).
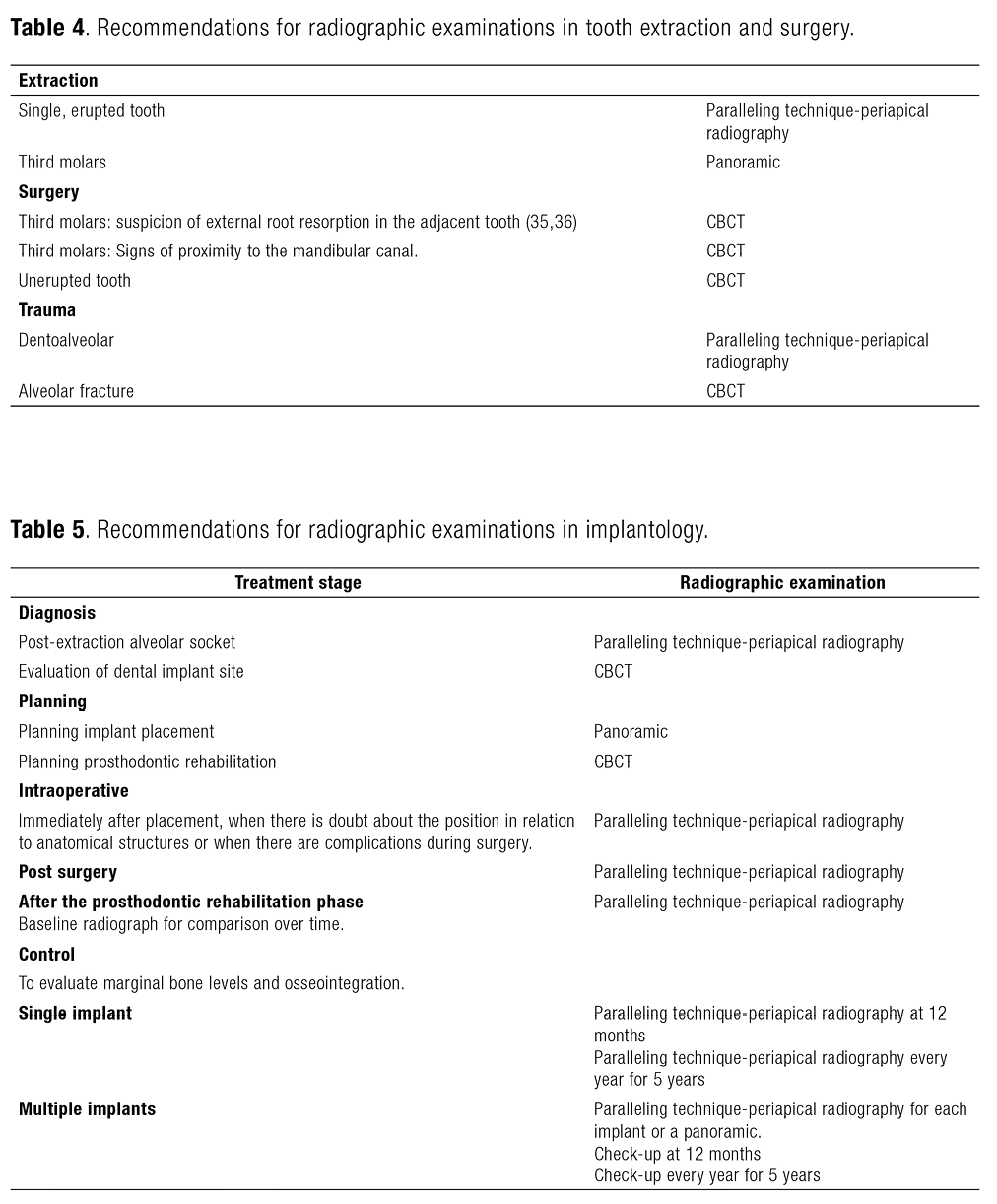
3. Radiographic diagnosis in periodontal evaluation
The goal of diagnosing the periodontal disease is to identify its stage and severity (15, 31, 32), considering the depth of the probe, the loss of insertion, the extent of bone loss, the presence of bone defects, and furcation lesions (32). There is no evidence to establish the periodic acquisition radiographs for periodontal evaluation (15).
Panoramic radiographs, the bisecting technique, and the adhesive bitewing technique are not recommended due to due to their inherent technical limitations (15, 32).
Although panoramic radiographs and the complete set of periapical radiographs have been used for periodontal evaluation, it is currently recommended to avoid this practice due to the limitations of panoramic radiographs and the fact that it involves a higher dose of radiation to the patient (15, 32) (Table 3).
4. Radiographic diagnosis in surgery
Surgical treatment requires appropriate diagnostic tests, which include radiographic imaging (34-37). Minor procedures are detailed below. Major surgeries are not considered, as they are performed by specialists in a hospital setting (Table 4).
5. Radiographic diagnosis of implants
X-rays are crucial for assessing the quantity and quality of bone, as well as their relation to the position and design of prosthetic rehabilitation (6, 15, 34).
While CBCT is indicated for treatment planning, the entire acquired tomographic volume must be evaluated and its findings documented in the patient's record (Table 5).
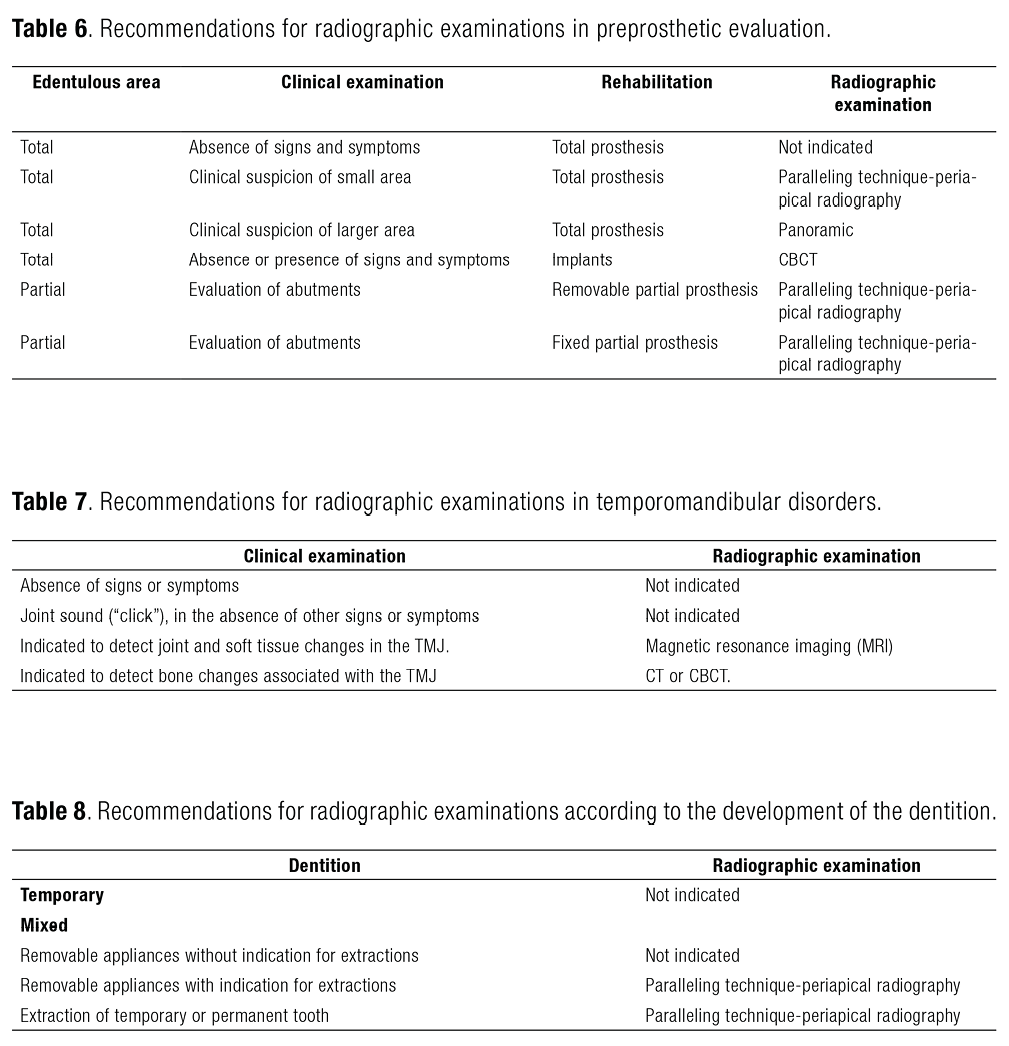
6. Radiographic diagnosis of edentulous bone ridge
The request for radiographic evaluation is based on the clinical signs or symptoms and the treatment to be performed. In the absence of clinical signs and symptoms, taking x-rays is not justified (15, 26) (Table 6).
7. Radiographic diagnosis of temporomandibular disorders (TMD)
The initial evaluation of TMD is based on the clinical examination of the TMJ region and the masticatory system (38). The request for a radiographic examination is based on the result of the clinical evaluation, when the evaluation of the bone component is required (15, 38) (Table 7).
8. Radiographic diagnosis of the development of the dentition
Figure 2, Figure 3, Figure 4 detail specific procedures for developing dentition, and do not include orthodontic treatments performed by specialists (15, 17) (Table 8).
CONCLUSIONS
Radiographic images are an essential diagnostic tool that should be employed only after a comprehensive history and clinical evaluation. Their use must be justified, as each type of intraoral and extraoral radiographic study-whether two-dimensional or three-dimensional-serves specific diagnostic purposes. It is crucial to carefully consider the limitations of each radiographic technique, as well as the effects of projection phenomena and reconstruction processes on the resulting images.
Given the rapid advancements in oral radiology, it is imperative to continuously update the criteria for imaging indications in dentistry based on the latest scientific evidence. This proactive approach not only enhances diagnostic accuracy but also prioritizes the well-being of patients and supports clinicians in their practice.
Author contribution statement
Conceptualization and design: L.B.R, A.C.R.I. and D.C.S
Literature review: L.B.R., A.C.R.I. and D.C.S.
Formal analysis: L.B.R., A.C.R.I. and D.C.S.
Writing-original draft preparation: L.B.R., A.C.R.I. and D.C.S.
Writing-review & editing: L.B.R., A.C.R.I. and D.C.S.
Supervision: L.B.R.
REFERENCIAS
1. Kim I.H., Singer S.R., Hong D.J., Mupparapu M. Fundamentals of Radiographic Interpretation for the Dentist. Dent Clin North Am. 2021; 65 (3): 409-25.
2. Jain S., Choudhary K., Nagi R., Shukla S., Kaur N., Grover D. New evolution of cone-beam computed tomography in dentistry: Combining digital technologies. Imaging Sci Dent. 2019; 49 (3): 179-90.
3. Gaêta-Araujo H., Alzoubi T., Vasconcelos K. de F., Orhan K., Pauwels R., Casselman J.W., et al. Cone beam computed tomography in dentomaxillofacial radiology: a two-decade overview. Dentomaxillofac Radiol. 2020; (20200145).
4. Nemtoi A., Czink C., Haba D., Gahleitner A. Cone beam CT: a current overview of devices. Dentomaxillofac Radiol. 2013; 42 (8): 20120443.
5. ICRP. Radiological Protection in Cone Beam Computed Tomography (CBCT). ICRP Publication 129. Ann ICRP. 2015; 44 (1): 9-127.
6. Consortium SEDENTEXCT, Horner K., Lindh C., Birch S., Christell H. Cone Beam CT for Dental and Maxillofacial Radiology: Evidence Based Guidelines, Radiation Protection Publication 172. 2012. 156 p.
7. ICRP. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37 (2-4): 1-332.
8. Horner K., O’Malley L., Taylor K., Glenny A.M. Guidelines for clinical use of CBCT: a review. Dentomaxillofac Radiol. 2015; 44 (1): 20140225.
9. Fryback D.G., Thornbury J.R. The efficacy of diagnostic imaging. Med Decis Making. 1991; 11 (2): 88-94.
10. Arancibia B., Schilling J., Schilling A., Correa-Beltrán G., Hidalgo A. Usos de tomografía computarizada de haz cónico en menores de 25 años en Talca, Chile. Rev Cubana Estomatol. 2017; 54 (3).
11. Barba L., Berrocal A.L., Hidalgo A. Uses of cone-beam computed tomography in San José, Costa Rica. Imaging Sci Dent. 2018; 48 (2): 103-9.
12. Hidalgo-Rivas J.A., Theodorakou C., Carmichael F., Murray B., Payne M., Horner K. Use of cone beam CT in children and young people in three United Kingdom dental hospitals. Int J Paediatr Dent. 2014; 24 (5): 336-48.
13. Barba Ramírez L., Ruiz García de Chacón V., Hidalgo Rivas A. El uso de rayos X en odontología y la importancia de la justificación de exámenes radiográficos. Avances en Odontoestomatología. 2020; 36 (3): 131-42.
14. Jacobs R., Fontenele R.C., Lahoud P., Shujaat S., Bornstein M.M. Radiographic diagnosis of periodontal diseases-Current evidence versus innovations. Periodontology 2000. 2024; 95 (1): 51-69.
15. Horner K., Eaton K.A. Selection Criteria for Dental Radiography. 3.a ed. London, UK: Faculty of General Dental Practice UK; 2018.
16. Salvi G.E., Roccuzzo A., Imber J.C., Stähli A., Klinge B., Lang N.P. Clinical periodontal diagnosis. Periodontology 2000. 2023; 1-19.
17. Isaacson K.G., Thom A.R., Atack N.E., Horner K., Whaites E. Guidelines for the Use of Radiographs in Clinical Orthodontics. 4.a ed. Vol. 31. London, UK: British Orthodontic Society; 2015.
18. Patel S., Brown J., Semper M., Abella F., Mannocci F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int Endod J. 2019; 52 (12): 1675-8.
19. Waite S., Scott J.M., Legasto A., Kolla S., Gale B., Krupinski E.A. Systemic Error in Radiology. AJR Am J Roentgenol. 2017; 209 (3): 629-39.
20. Ortega T.D., García M.C. Prevención de riesgo en radiología: el error y el radiólogo. Revista chilena de radiología. 2002; 8 (3): 135-40.
21. Hegde S., Gao J., Vasa R., Cox S. Factors affecting interpretation of dental radiographs. Dentomaxillofac Radiol. 2023; 52 (2): 20220279.
22. Waite S., Scott J., Gale B., Fuchs T., Kolla S., Reede D. Interpretive Error in Radiology. Am J Roentgenol. 2017; 208 (4): 739-49.
23. Waite S., Grigorian A., Alexander R.G., Macknik S.L., Carrasco M., Heeger D.J., et al. Analysis of Perceptual Expertise in Radiology-Current Knowledge and a New Perspective. Front Hum Neurosci. 2019; 13.
24. Hegde S., Nanayakkara S., Cox S., Vasa R., Gao J. Australian Dentists’ Knowledge of the Consequences of Interpretive Errors in Dental Radiographs and Potential Mitigation Measures. Clin Exp Dent Res. 2024; 10 (6): e70027.
25. Robinson P.J. Radiology’s Achilles’ heel: error and variation in the interpretation of the Röntgen image. Br J Radiol. 1997; 70 (839): 1085-98.
26. Horner K., Rushton V.E., Walker A., Tsiklaskis K., Hirschmann P., Van der S.P., et al. European Commission. Radiation Protection136. European Guidelines on Radiation Protection in Dental Radiology. The safe use of radiographs in dental practice. Luxembourg Office for Official Publications of the European Communities.
27. European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006; 39 (12): 921-30.
28. Stera G., Giusti M., Magnini A., Calistri L., Izzetti R., Nardi C. Diagnostic accuracy of periapical radiography and panoramic radiography in the detection of apical periodontitis: a systematic review and meta-analysis. Radiol Med. 2024; (11): 1682-1695. doi: 10.1007/s11547-024-01882-z.
29. Rosen E., Salem R., Kavalerchik E., Kahn A., Tsesis I. The effect of imaging modality on the evaluation of the outcome of endodontic surgery. Dentomaxillofac Radiol. 2022; 51 (8): 20220164.
30. Chugal N., Assad H., Markovic D., Mallya S.M. Applying the American Association of Endodontists and American Academy of Oral and Maxillofacial Radiology guidelines for cone-beam computed tomography prescription: Impact on endodontic clinical decisions. J Am Dent Assoc. 2024; 155 (1): 48-58.
31. Choi I.G.G., Cortes A.R.G., Arita E.S., Georgetti M.A.P. Comparison of conventional imaging techniques and CBCT for periodontal evaluation: A systematic review. Imaging Sci Dent. 2018; 48 (2): 79-86.
32. Jacobs, R.; Fontenele, R.C.; Lahoud, P.; Shujaat, S.; Bornstein, M.M. Radiographic diagnosis of periodontal diseases - Current evidence versus innovations. Periodontology 2000. 2024; 95 (1): 51-69.
33. Haas L.F., Zimmermann G.S., De Luca Canto G, Flores-Mir C, Corrêa M. Precision of cone beam CT to assess periodontal bone defects: a systematic review and meta-analysis. Dentomaxillofac Radiol. 2018; 47 (2): 20170084.
34. Wang S., Ford B. Imaging in Oral and Maxillofacial Surgery. Dent Clin North Am. 2021; 65 (3): 487-507.
35. Reia V.C.B., de Toledo Telles-Araujo G., Peralta-Mamani M., Biancardi M.R., Rubira C.M.F., Rubira-Bullen I.R.F. Diagnostic accuracy of CBCT compared to panoramic radiography in predicting IAN exposure: a systematic review and meta-analysis. Clin Oral Investig. 2021; 25 (8): 4721-33.
36. Moreira-Souza L., Butini Oliveira L., Gaêta-Araujo H., Almeida-Marques M., Asprino L., Oenning A.C. Comparison of CBCT and panoramic radiography for the assessment of bone loss and root resorption on the second molar associated with third molar impaction: a systematic review. Dentomaxillofac Radiol. 2022; 51 (3): 20210217.
37. Matzen L.H., Schropp L., Spin-Neto R., Wenzel A. Radiographic signs of pathology determining removal of an impacted mandibular third molar assessed in a panoramic image or CBCT. Dentomaxillofac Radiol. 2017; 46 (1): 20160330.
38. Schroder Â.G.D., Gonçalves F.M., Germiniani J. da S., Schroder L.D., Porporatti A.L., Zeigelboim B.S., et al. Diagnosis of TMJ degenerative diseases by panoramic radiography: is it possible? A systematic review and meta-analysis. Clin Oral Investig. 2023; 27 (11): 6395-412.