Abstract
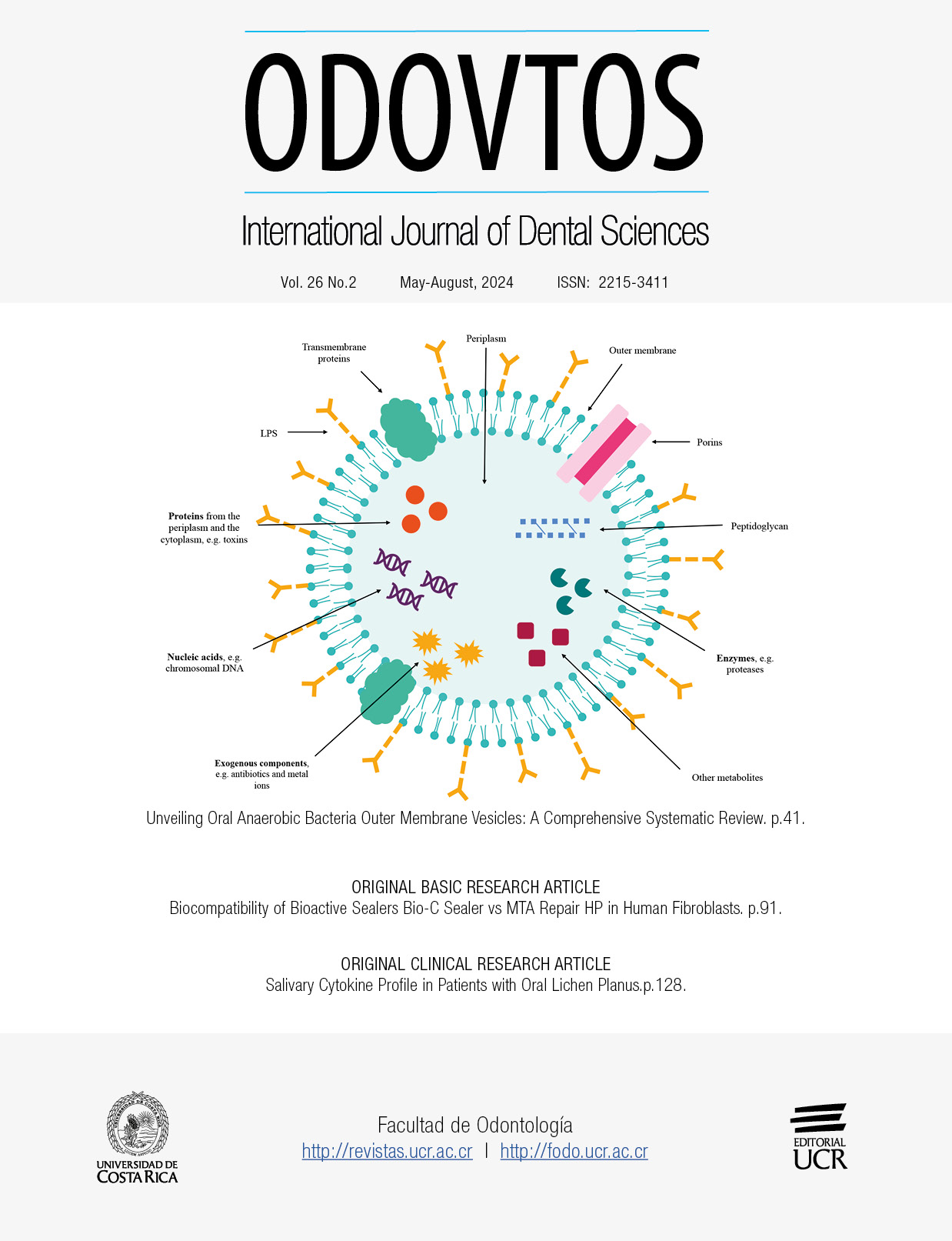
Extracellular vesicles (EV) are spherical structures limited by membranes and shed by several cell types. Specifically, outer membrane vesicles (OMVs) are nanometric particles constitutively produced by Gram-negative bacteria (GNB) under different environmental conditions. OMVs are biologically active; they are loaded with selected lipids, polysaccharides, proteins, and even different types of nucleic acids. OMVs from pathogenic oral bacteria play key roles in pathogen-host interactions, constituting a possible link between oral health and systemic disease. OMVs participate in adhesion, invasion, and damage to cells, as well as in modulating the host's immune response, biofilm formation, and promotion of virulence. The objective of this systematic review was to collect, analyze and synthesize the knowledge available on literature reviews on OMVs of the most studied pathogenic oral anaerobic GNB. This information was classified into the following categories: induction of vesiculation and biogenesis, its liberation from the parental cell, content, internalization by another host cell, and the interaction with the host cell. It was found that the most studied OMVs are those of Porphyromonas gingivalis and Bacteroides spp. and, to a lesser extent, Aggregatibacter spp., and Treponema spp. This systematic review provides a synthesis of the current knowledge regarding OMVs, with emphasis on the information available for periodontopathogens.
References
Barboza-Solís C., Acuña-Amador L. The Oral Microbiota: A Literature Review for Updating Professionals in Dentistry. Part I. Odovtos-International Journal of Dental Sciences. 2019 Oct 1; 22 (1): 143-52.
Barboza-Solís, C., & Acuña-Amador, L. A. (2021). The oral microbiota: A literature review for updating profesional s in dentistry-Part II. Odovtos International Journal of Dental Sciences, 23 (3), 45-56. http://dx.doi.org/10.15517/ijds.2021.45330
Holt S.C., Ebersole J.L. Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia: the ‘red complex’, a prototype polybacterial pathogenic consortium in periodontitis. Periodontol 2000. 2005 Jun 21; 38 (1): 72-122.
da Silva-Boghossian C.M., do Souto R.M., Luiz R.R., Colombo A.P.V. Association of red complex, A. actinomycetemcomitans and non-oral bacteria with periodontal diseases. Arch Oral Biol. 2011 Sep; 56 (9): 899-906.
Buonavoglia A., Latronico F., Pirani C., Greco M.F., Corrente M., Prati C. Symptomatic and asymptomatic apical periodontitis associated with red complex bacteria: clinical and microbiological evaluation. Odontology. 2013 Jan 6; 101 (1): 84-8.
Suzuki, N., Yoneda, M., & Hirofuji, T. (2013). Mixed red-complex bacterial infection in periodontitis. International journal of dentistry, 2013. https://doi.org/10.1155/2013/587279
Lanza E., Magan-Fernandez A., Bermejo B., de Rojas J., Marfil-Alvarez R., Mesa F. Complementary clinical effects of red complex bacteria on generalized periodontitis in a caucasian population. Oral Dis. 2016 Jul 26; 22 (5): 430-7.
Mahendra J., Mahendra L., Sharma V., Alamoudi A., Bahammam H.A., Mugri M.H., et al. Red-Complex Bacterial Levels in Pregnant Women With Preeclampsia and Chronic Periodontitis. Int Dent J. 2023 Aug; 73 (4): 503-10.
Nagao, Y., & Tanigawa, T. (2019). Red complex periodontal pathogens are risk factors for liver cirrhosis. Biomedical reports, 11 (5): 199-206. https://doi.org/10.3892/br.2019.1245
Mahendra J., Mahendra L., Felix J., Romanos G.E. Genetic analysis of P orphyromonas gingivalis (fimA), Aggregatibacter actinomycetemcomitans, and red complex in coronary plaque. J Investig Clin Dent. 2014 Aug 27; 5 (3): 201-7.
Guo J., Lin K., Wang S., He X., Huang Z., Zheng M. Effects and mechanisms of Porphyromonas gingivalis outer membrane vesicles induced cardiovascular injury. BMC Oral Health. 2024 Jan;24(1):112.
Guo J., Lin K., Wang S., He X., Huang Z., Zheng M. Effects and mechanisms of Porphyromonas gingivalis outer membrane vesicles induced cardiovascular injury. BMC Oral Health. 2024 Jan; 24 (1): 112.
Ha J.Y., Seok J., Kim S.J., Jung H.J., Ryu K.Y., Nakamura M., et al. Periodontitis promotes bacterial extracellular vesicle-induced neuroinflammation in the brain and trigeminal ganglion. Philpott DJ, editor. PLoS Pathog. 2023 Oct; 19 (10): e1011743.
Wang, Z., Cui, L., Nan, Y., Liu, J., & Li, C. (2023). Periodontitis & preeclampsia: were outer membrane vesicles a potential connection?. The Journal of Maternal-Fetal & Neonatal Medicine, 36 (1): 2183767. https://doi.org/10.1080/14767058.2023.2183767
Visan K.S., Wu L.Y., Voss S., Wuethrich A., Möller A. Status quo of Extracellular Vesicle isolation and detection methods for clinical utility. Semin Cancer Biol. 2023 Jan; 88: 157-71.
Rayamajhi S., Sulthana S., Ferrel C., Shrestha T.B., Aryal S. Extracellular vesicles production and proteomic cargo varies with incubation time and temperature. Exp Cell Res. 2023 Jan; 422 (2): 113454.
Woith E., Fuhrmann G., Melzig M.F. Extracellular Vesicles-Connecting Kingdoms. Int J Mol Sci. 2019 Nov 14; 20 (22): 5695.
Brown L., Wolf J.M., Prados-Rosales R, Casadevall A. Through the wall: extracellular vesicles in Gram-positive bacteria, mycobacteria and fungi. Nat Rev Microbiol. 2015 Oct 1; 13 (10): 620-30.
Deatherage B.L., Cookson B.T. Membrane Vesicle Release in Bacteria, Eukaryotes, and Archaea: a Conserved yet Underappreciated Aspect of Microbial Life. Andrews-Polymenis HL, editor. Infect Immun. 2012 Jun; 80 (6): 1948-57.
Liebana-Jordan M., Brotons B., Falcon-Perez J.M., Gonzalez E. Extracellular Vesicles in the Fungi Kingdom. Int J Mol Sci. 2021 Jul 5; 22 (13): 7221.
Sabatke B., Gavinho B., Coceres V., de Miguel N., Ramirez M.I. Unveiling the role of EVs in anaerobic parasitic protozoa. Mol Immunol. 2021 May; 133: 34-43.
Lian M.Q., Chng W.H., Liang J., Yeo H.Q., Lee C.K., Belaid M., et al. Plant-derived extracellular vesicles: Recent advancements and current challenges on their use for biomedical applications. J Extracell Vesicles. 2022 Dec 15; 11 (12): 12283.
Lin C., Guo J., Jia R. Roles of Regulatory T Cell-Derived Extracellular Vesicles in Human Diseases. Int J Mol Sci. 2022 Sep 23; 23 (19): 11206.
Liu J., Cvirkaite-Krupovic V., Commere P.H., Yang Y., Zhou F., Forterre P., et al. Archaeal extracellular vesicles are produced in an ESCRT-dependent manner and promote gene transfer and nutrient cycling in extreme environments. ISME J. 2021 Oct 26; 15 (10): 2892-905.
Ñahui Palomino R.A., Vanpouille C., Costantini P.E., Margolis L. Microbiota-host communications: Bacterial extracellular vesicles as a common language. Oh J, editor. PLoS Pathog. 2021 May 13; 17 (5): e1009508.
Chen, J., Zhang, H., Wei, B., Wu, Q., & Wang, H. (2022). Inhibitors of bacterial extracellular vesicles. Frontiers in Microbiology, 13: 835058. https://doi.org/10.3389/fmicb.2022.835058
Gupta, S., & Rodriguez, G. M. (2018). Mycobacterial extracellular vesicles and host pathogen interactions. Pathogens and disease, 76 (4): fty031. doi: 10.1093/femspd/fty031
O’Donoghue E.J., Krachler A.M. Mechanisms of outer membrane vesicle entry into host cells. Cell Microbiol. 2016 Nov; 18 (11): 1508-17.
Gill S., Catchpole R., Forterre P. Extracellular membrane vesicles in the three domains of life and beyond. FEMS Microbiol Rev. 2019 May 1; 43 (3): 273-303.
Cao Y., Lin H. Characterization and function of membrane vesicles in Gram-positive bacteria. Appl Microbiol Biotechnol. 2021 Mar 6; 105 (5): 1795-801.
Pérez-Cruz C., Delgado L., López-Iglesias C., Mercade E. Outer-Inner Membrane Vesicles Naturally Secreted by Gram-Negative Pathogenic Bacteria. Rudel T, editor. PLoS One. 2015 Jan 12; 10 (1): e0116896.
Castillo-Romero K.F., Santacruz A., González-Valdez J. Production and purification of bacterial membrane vesicles for biotechnology applications: Challenges and opportunities. Electrophoresis. 2023 Jan; 44 (1-2): 107-24.
van der Pol E., Böing A.N., Gool E.L., Nieuwland R. Recent developments in the nomenclature, presence, isolation, detection and clinical impact of extracellular vesicles. Journal of Thrombosis and Haemostasis. 2016 Jan;14 (1): 48-56.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., & Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 372. https://doi.org/10.1136/bmj.n71
Ofir-Birin Y., Heidenreich M., Regev-Rudzki N. Pathogen-derived extracellular vesicles coordinate social behaviour and host manipulation. Semin Cell Dev Biol. 2017 Jul; 67: 83-90.
Bonnington K.E., Kuehn M.J. Protein selection and export via outer membrane vesicles. Biochimica et Biophysica Acta (BBA)- Molecular Cell Research. 2014 Aug; 1843 (8): 1612-9.
Jahromi L.P., Fuhrmann G. Bacterial extracellular vesicles: Understanding biology promotes applications as nanopharmaceuticals. Adv Drug Deliv Rev. 2021 Jun; 173: 125-40.
Klimentová J., Stulík J. Methods of isolation and purification of outer membrane vesicles from gram-negative bacteria. Microbiol Res. 2015 Jan; 170: 1-9.
Lécrivain A.L., Beckmann B.M. Bacterial RNA in extracellular vesicles: A new regulator of host-pathogen interactions? Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms. 2020 Jul; 1863 (7): 194519.
Ma, L., & Cao, Z. (2021). Membrane vesicles from periodontal pathogens and their potential roles in periodontal disease and systemic illnesses. Journal of Periodontal Research, 56 (4): 646-655. https://doi.org/10.1111/jre.12884
Baker J.L., Chen L., Rosenthal J.A., Putnam D., DeLisa M.P. Microbial biosynthesis of designer outer membrane vesicles. Curr Opin Biotechnol. 2014 Oct; 29 (1): 76-84.
Jiang L., Schinkel M., van Essen M., Schiffelers R.M. Bacterial membrane vesicles as promising vaccine candidates. European Journal of Pharmaceutics and Biopharmaceutics. 2019 Dec; 145 (September):1-6.
Doré E., Boilard E. Bacterial extracellular vesicles and their interplay with the immune system. Pharmacol Ther. 2023 Jul; 247: 108443.
Long Q., Zheng P., Zheng X., Li W., Hua L., Yang Z., et al. Engineered bacterial membrane vesicles are promising carriers for vaccine design and tumor immunotherapy. Adv Drug Deliv Rev. 2022 Jul; 186: 114321.
Amano A., Takeuchi H., Furuta N. Outer membrane vesicles function as offensive weapons in host-parasite interactions. Microbes Infect. 2010 Oct; 12 (11): 791-8.
Miller S.I., Bader M., Guina T. Bacterial Vesicle Formation as a Mechanism of Protein Transfer to Animals. Cell. 2003 Oct; 115 (1): 2-3.
Toyofuku M., Tashiro Y., Hasegawa Y., Kurosawa M., Nomura N. Bacterial membrane vesicles, an overlooked environmental colloid: Biology, environmental perspectives and applications. Adv Colloid Interface Sci. 2015 Dec; 226: 65-77.
Huang J., Wang X., Wang Z., Deng L., Wang Y., Tang Y., et al. Extracellular vesicles as a novel mediator of interkingdom communication. Cytokine Growth Factor Rev. 2023 Oct; 73: 173-84.
Pumbwe L., Skilbeck C.A., Wexler H.M. The Bacteroides fragilis cell envelope: Quarterback, linebacker, coach-or all three? Anaerobe. 2006 Oct; 12 (5-6): 211-20.
Gurunathan S., Kim J.H. Bacterial extracellular vesicles: Emerging nanoplatforms for biomedical applications. Microb Pathog. 2023 Oct; 183: 106308.
Domingues S., Nielsen K.M. Membrane vesicles and horizontal gene transfer in prokaryotes. Curr Opin Microbiol. 2017 Aug; 38:1 6-21.
Gnopo Y.M.D., Watkins H.C., Stevenson T.C., DeLisa M.P., Putnam D. Designer outer membrane vesicles as immunomodulatory systems-Reprogramming bacteria for vaccine delivery. Adv Drug Deliv Rev. 2017 May; 114: 132-42.
Gui M.J., Dashper S.G., Slakeski N., Chen Y.Y., Reynolds E.C. Spheres of influence: Porphyromonas gingivalis outer membrane vesicles. Mol Oral Microbiol. 2016 Oct; 31 (5): 365-78.
Schuh C.M.A.P., Cuenca J., Alcayaga-Miranda F., Khoury M. Exosomes on the border of species and kingdom intercommunication. Translational Research. 2019 Aug; 210: 80-98.
Li D., Zhu L., Wang Y., Zhou X., Li Y. Bacterial outer membrane vesicles in cancer: Biogenesis, pathogenesis, and clinical application. Biomedicine & Pharmacotherapy. 2023 Sep; 165: 115120.
Xie H. Biogenesis and function of Porphyromonas gingivalis outer membrane vesicles. Future Microbiol. 2015 Sep 1; 10 (9): 1517-27.
Xie J., Li Q., Nie S. Bacterial extracellular vesicles: An emerging postbiotic. Trends Food Sci Technol. 2024 Jan; 143: 104275.
Zhang Z., Liu D., Liu S., Zhang S., Pan Y. The Role of Porphyromonas gingivalis Outer Membrane Vesicles in Periodontal Disease and Related Systemic Diseases. Front Cell Infect Microbiol. 2021 Jan 28; 10 (January): 1-12.
Shen Q., Xu B., Wang C., Xiao Y, Jin Y. Bacterial membrane vesicles in inflammatory bowel disease. Life Sci. 2022 Oct; 306: 120803.
Xie J., Haesebrouck F., Van Hoecke L., Vandenbroucke R.E. Bacterial extracellular vesicles: an emerging avenue to tackle diseases. Trends Microbiol. 2023 Dec; 31 (12): 1206-24.
Zhao Y., Li X., Zhang W., Yu L., Wang Y., Deng Z., et al. Trends in the biological functions and medical applications of extracellular vesicles and analogues. Acta Pharm Sin B. 2021 Aug;1 1 (8): 2114-35.
Tsatsaronis J.A., Franch-Arroyo S., Resch U., Charpentier E. Extracellular Vesicle RNA: A Universal Mediator of Microbial Communication? Trends Microbiol. 2018 May; 26 (5): 401-10.
Dhital, S., Deo, P., Stuart, I., & Naderer, T. (2021). Bacterial outer membrane vesicles and host cell death signaling. Trends in Microbiology, 29 (12): 1106-1116. https://doi.org/10.1016/j.tim.2021.04.003
Ebner P., Götz F. Bacterial Excretion of Cytoplasmic Proteins (ECP): Occurrence, Mechanism, and Function. Trends Microbiol. 2019 Feb; 27 (2): 176-87.
Wu Q.Y., Liu B.C., Ruan X.Z., Ma K.L. Intestinal microbiota-derived membrane vesicles and their role in chronic kidney disease. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2022 Oct; 1868 (10): 166478.
Liu H., Li M., Zhang T., Liu X., Zhang H., Geng Z., et al. Engineered bacterial extracellular vesicles for osteoporosis therapy. Chemical Engineering Journal. 2022 Dec; 450: 138309.
Barteneva N.S., Baiken Y., Fasler-Kan E., Alibek K., Wang S., Maltsev N., et al. Extracellular vesicles in gastrointestinal cancer in conjunction with microbiota: On the border of Kingdoms. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer. 2017 Dec;1868 (2): 372-93.
Tsai Y.L., Tsai W.C., Qing Z., Chang C.J. Dichotomous effects of microbial membrane vesicles on the regulation of immunity. Medicine in Microecology. 2020 Mar; 3 (April): 100009.
Okamura H., Hirota K., Yoshida K., Weng Y., He Y., Shiotsu N., et al. Outer membrane vesicles of Porphyromonas gingivalis: Novel communication tool and strategy. Japanese Dental Science Review. 2021 Nov; 57: 138-46.
Mehanny M., Lehr C.M., Fuhrmann G. Extracellular vesicles as antigen carriers for novel vaccination avenues. Adv Drug Deliv Rev. 2021 Jun; 173: 164-80.
Tanai A., Okamura H. The role of extracellular vesicles throughout normal pregnancy and in relation to oral bacteria. J Oral Biosci. 2021 Mar; 63 (1): 14-22.
Van der Ley P., Schijns V.E. Outer membrane vesicle-based intranasal vaccines. Curr Opin Immunol. 2023 Oct; 84: 102376.
Ahmed A.A.Q., McKay T.J.M. Environmental and ecological importance of bacterial extracellular vesicles (BEVs). Science of The Total Environment. 2024 Jan; 907: 168098.
Xie J., Li Q., Nie S. Bacterial extracellular vesicles: An emerging postbiotic. Trends Food Sci Technol. 2024 Jan; 143: 104275.
Aytar Çelik P., Derkuş B., Erdoğan K., Barut D., Blaise Manga E., Yıldırım Y., et al. Bacterial membrane vesicle functions, laboratory methods, and applications. Biotechnol Adv. 2022 Jan; 54: 107869.
Huang W., Meng L., Chen Y., Dong Z., Peng Q. Bacterial outer membrane vesicles as potential biological nanomaterials for antibacterial therapy. Acta Biomater. 2022 Mar; 140: 102-15.
Stentz R., Carvalho A.L., Jones E.J., Carding S.R. Fantastic voyage: the journey of intestinal microbiota-derived microvesicles through the body. Biochem Soc Trans. 2018 Oct 19;46 (5): 1021-7.
Tiku V., Tan M.W. Host immunity and cellular responses to bacterial outer membrane vesicles. Trends Immunol. 2021 Nov; 42 (11): 1024-36.
Ji N., Wang F., Wang M., Zhang W., Liu H., Su J. Engineered bacterial extracellular vesicles for central nervous system diseases. Journal of Controlled Release. 2023 Dec; 364: 46-60.
Niu G., Jian T., Gai Y., Chen J. Microbiota and plant-derived vesicles that serve as therapeutic agents and delivery carriers to regulate metabolic syndrome. Adv Drug Deliv Rev. 2023 May;196:114774.
Fuhrmann G., Neuer A.L., Herrmann I.K. Extracellular vesicles – A promising avenue for the detection and treatment of infectious diseases? European Journal of Pharmaceutics and Biopharmaceutics. 2017 Sep; 118: 56-61.
Chen L., Ou Q., Kou X. Extracellular vesicles and their indispensable roles in pathogenesis and treatment of inflammatory bowel disease: A comprehensive review. Life Sci. 2023 Aug; 327: 121830.
Dong X., Liu Y., Yang X., Li T. Extracellular vesicle miRNAs as key mediators in diet-gut microbiome-host interplay. Trends Food Sci Technol. 2023 Jun; 136: 268-81.
Liu H., Zhang Q., Wang S., Weng W., Jing Y., Su J. Bacterial extracellular vesicles as bioactive nanocarriers for drug delivery: Advances and perspectives. Bioact Mater. 2022 Aug;14: 169-81.
Moloudizargari M., Asghari M.H., Goel A. The therapeutic triad of extracellular vesicles: As drug targets, as drugs, and as drug carriers. Biochem Pharmacol. 2021 Oct; 192: 114714.
Wang D., Guan S., Lu P., Li Y., Xu H. Extracellular vesicles: Critical bilateral communicators in periphery-brain crosstalk in central nervous system disorders. Biomedicine & Pharmacotherapy. 2023 Apr; 160: 114354.
Díez-Sainz E., Milagro F.I., Riezu-Boj J.I., Lorente-Cebrián S. Effects of gut microbiota–derived extracellular vesicles on obesity and diabetes and their potential modulation through diet. J Physiol Biochem. 2022 May 2; 78 (2): 485-99.
Song M., Cui M., Fang Z., Liu K. Advanced research on extracellular vesicles based oral drug delivery systems. Journal of Controlled Release. 2022 Nov; 351: 560-72.
Xie J., Li Q., Haesebrouck F., Van Hoecke L., Vandenbroucke R.E. The tremendous biomedical potential of bacterial extracellular vesicles. Trends Biotechnol. 2022 Oct; 40 (10): 1173-94.
##plugins.facebook.comentarios##

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Copyright (c) 2024 Priscilla Castro-Vargas, Frédérique Barloy-Hubler, Luis Acuña-Amador